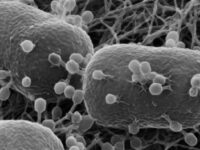
The only place that prioritizes its department of defense more than the United States is the human body. We have a comprehensive immune system with two lines of protection: barriers and fighters. Within this second line of defense, antibodies act as soldiers that circle through the bloodstream marking foreign invaders for destruction.
Specifically, the immune system’s internal army consists of many types of white blood cells, such as B cells, T cells, and macrophages that work together to recognize and destroy pathogens. B cells, with assistance from helper T cells, create antibodies. Antibodies are Y-shaped proteins that connect to antigens, unique markers carried by pathogens. Some antibodies directly disarm the invader while others cause macrophages to engulf it or signal killer T cells to initiate cell death of infected cells.
New therapies are taking advantage of the strategy our bodies already have in place for attacking pathogens. Physicians can now send in more troops to help fight off various diseases, from type 1 diabetes to Alzheimer’s, using monoclonal antibodies.
“While this technology has been around since 1975, applications of these artificial antibodies have diversified in the past few years.”
Monoclonal antibodies are essentially artificial antibodies designed to target specific cells or viruses by binding to a particular antigen carried on their surfaces. To produce these molecules in bulk, scientists inject lab mice with the target antigen. Then, they isolate the B cells from the animal and fuse them with tumor cells, resulting in hybrid cells that produce the desired antibody and divide indefinitely. Originating from a single B cell, each daughter cell produces identical antibodies, clones that only bind to the target antigen.
“Physicians can now send in more troops to help fight off various diseases, from type 1 diabetes to Alzheimer’s, using monoclonal antibodies.”
While this technology has been around since 1975, applications of these artificial antibodies have diversified in the past few years. One exciting treatment uses monoclonal antibodies to defer the onset of type 1 diabetes symptoms. Second only to asthma, type 1 diabetes is one of the most prevalent childhood illnesses, and this is the first time there is any available preventative therapy. In type 1 diabetes, the body’s immune system turns against cells in the pancreas that normally produce insulin. If a child could have two extra years before developing the disorder, they could spend 730 more days without testing their blood sugar every few hours, injecting themselves with expensive exogenous insulin, and worrying about mistakes sending them to the emergency room. The new infusion treatment Teplizumab (the suffix “mab” refers to monoclonal antibody) offers just that.
Teplizumab is a medication traditionally used to prevent organ recipients from rejecting transplants. The drug likely works by binding to receptors on the surface of T cells, preventing the cells from recognizing and destroying their targets.
Patients must be diagnosed before symptoms of blood sugar imbalances begin in order to qualify for this intervention. Siblings of patients who are already living with diabetes make up a large portion of the drug’s recipients as they have reason to get tested for autoantibodies and are more often diagnosed before they progress to a symptomatic stage.
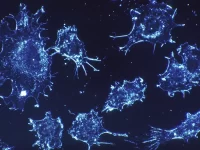
Scientists have also been working on Alzheimer’s treatments using monoclonal antibodies. This research focuses on beta-amyloid plaques, which are buildups in the brain believed to be responsible for the cognitive decline seen in Alzheimer’s patients. Targeted monoclonal antibodies bind to these beta-amyloid plaques and recruit white blood cells to destroy them.
There are several monoclonal antibody drugs for Alzheimer’s disease available today, though none of them are miracle cures. In a two-year study on Gantenerumab by Roche Pharma, the drug was found to reduce the amount of beta-amyloid plaques to below the “amyloid-beta positivity threshold” in 51% of participants. This means that their brain scans would not indicate a clinical diagnosis of Alzheimer’s disease. Unfortunately, later phases of Gantenerumab testing found no clinically significant reduction in cognitive decline. This situation repeated itself with Biogen’s Aducanumab trial at the end of 2019, which ended prematurely because the data suggested futile chances of participants gaining significant quality-of-life improvement despite the reduction in beta-amyloid plaques. Unlike these outcomes, the most recent Alzheimer’s monoclonal antibody drug, Lecanemab, was shown to slow cognitive decline moderately, which pushed the FDA to grant accelerated approval of this drug on Jan. 6 of this year.
Our bodies are armed with fighters of disease, eager to combat invaders and traitors. Harnessing the power of our body’s own defense system is bringing hope to those with some of the most devastating and previously unconquerable diseases. Monoclonal antibodies are just scratching the surface of the potential cures we may discover by directing white blood cells to fight their own battles.
Image courtesy of Pixabay