Even after three long years, COVID-19 continues to sweep through the world’s population. Testing positive is detrimental to many, preventing those infected from going to work and providing for their family. With the effects of COVID-19, it is hard to imagine what having extended symptoms would be like. Recently, many have been reporting that they are experiencing long-term loss of smell. Though often overlooked, smell plays a big role in daily life. Smells can provoke distant memories, improve mood, and allow us to taste. Without smell, life — and food — seem bland; this is the life of some after getting COVID-19.
The symptoms of COVID-19 include fatigue, fever, shortness of breath, congestion, sore throat, and many more. One that many find concerning is a loss of smell. While many were able to regain their sense of smell as they recovered from their infection, some have reported long-term loss of smell. Reasons behind the prolonged symptom became the focus of researchers from Harvard Medical School, Duke Health, and the University of California, San Diego. In a recent study, they found that those with long-term loss of smell experience long-term immune responses in their olfactory (smell) nerve cells.
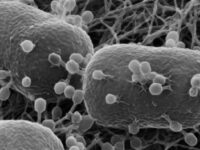
These teams of researchers found that the COVID-19 virus targeted olfactory sensory neurons. After an olfactory biopsy analysis where a collection of olfactory skin was examined, researchers found high numbers of T cells, a type of white blood cell that aids the immune system in fighting infections, in an inflammatory response despite no COVID-19 detection. The reason for the extended inflammatory response is unknown, though a potential justification is that it involves increased protection and repair of the skin barrier function. As a result, the researchers predicted that this long-term, ongoing inflammatory response is the cause of the decrease in olfactory sensory neurons, causing the long-term loss of smell.
There is still no definitive reason as to why some people experience long-term smell loss and others do not; however, there have been some hypothesized roots. These researchers produced three predictions: a lack of stem cell pools for skin repair, the overpopulation of T cells disrupting normal cell function, and changes to the olfactory cortex.
One, severe damage to the olfactory epithelium causes large numbers of stem cell pools to lessen. These stem cell pools allow the skin to renew following injury, so the lack of such cells would inhibit the regrowth of new olfactory epithelium and thus result in a loss of smell.
Two, the influx of T cells and other immune cell populations to the olfactory epithelium disturbs normal function of the cells through changes in gene expression. Long-term inflammatory responses are not healthy for cells and can lead to changes in the gene expression and possibly cell function.
And three, there could be alterations to the gene expression in the olfactory bulbs or olfactory cortex. Such changes can be fatal to an individual’s sense of smell, as derangements of the neurons in the brain can result in a long-term loss of smell.
Such research and identification of what sites are damaged and what cell types are present is important in the development of medications. A growth of more individualized medications can arise, allowing people to receive treatment tailored to their needs. Additionally, these recent breakthroughs highlight a need for further research and treatments for those with a loss of olfactory function. With this knowledge, scientists can apply these understandings to other long-term COVID-19 symptoms like fatigue, shortness of breath, and brain fog in advancing treatment methods and therapeutic applications. Advances in the medicine will promote scientists and doctors to handle viruses like COVID-19 better, allowing people to live their most healthy lives.
Image courtesy of Wikimedia Commons