After waking up from surgery, we tend to focus on if it was successful, if there is any pain, or if we embarrassed ourselves in front of the doctors. We rarely ask questions about the anesthesia used to put us under. Common surgeries and procedures ranging from root canals to childbirth use forms of anesthesia to reduce patient pain. No doubt anesthesia has been a large part of advancing treatment; without it, patients would shy away from treatment or be at risk while on the table. Regardless of use, is it safe? And for whom?
“Ironically, the medicine used to spare him pain was responsible for his fear.”
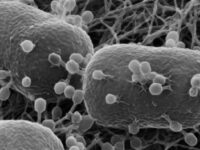
Cocktail therapy or not, anesthesia is a collection of medications, appropriately called anesthetics, that cause sedation or numbness. Anesthesia can be given in various ways: locally, generally, or spinally, with each kind affecting a larger area faster than the last. When administered locally, anesthetics are more numbing than sedating. Operations like root canals use local anesthetics, commonly Novocain, to numb the gum area. Five to ten minutes post-injection, the subcutaneous tissue will numb for under an hour and any pain signals in that area will be blocked from reaching your brain and creating an emotional response. Though a similar mechanism, general anesthesia leaves you unconscious which keeps your heart rate steady and blood loss controlled. Spinal anesthetics are injected directly into the cerebrospinal fluid, such as epidurals given during childbirth.
One of the earliest records of anesthesia dates back to 13th century Europe when physicians and apothecaries would use opium or alcohol-soaked sponges. In the early 1800s, US soldiers were still being given bullets to bite down on to undergo amputation. It wasn’t until 1846 at Massachusetts General Hospital that doctors William T. G. Morton and John Collins Warren used sulfuric ether to remove a tumor from a patient’s neck. Today, sulfuric ether has become outdated by anesthesiologists due to side effects such as spasms, mucosal membrane irritation, and smell.
Though sulfuric ether aged out, that doesn’t mean more modern mixtures are harmless. The kind of daze wisdom teeth extraction patients leave a clinic in has made for amusing videos, but what happens when a patient isn’t in the correct age group or is given too much? The phenomenon of perioperative delirium highlights the experience of patients — particularly older than 60 — experiencing lingering, disruptive effects due to anesthesia.
“The phenomenon of perioperative delirium highlights the experience of patients — particularly older than 60 — experiencing lingering, disruptive effects due to anesthesia.”
A study conducted through the University of Massachusetts Medical School, led by current Northeastern professor Jane Saczynski, found that elderly patients have a higher risk of delirium after being discharged. Participants were evaluated based on memory, recall, and attention. Those with perioperative delirium took between six months to a full year to return to their normal cognitive capabilities. Their symptoms can be characterized by brain fog, lasting either days or years, which puts them at risk of developing neurodegenerative disorders or decreased capacity for physical function. Eighty-one-year-old Professor Susan Baker underwent vertebrate surgery and woke up stable the following day. Later on, she reported hallucinations of looming fires and forgetfulness of her location and situation. Patients with pre-existing conditions are at an increased risk as well, specifically those with Alzheimer’s, Parkinson’s, or epilepsy. Seventy-six-year-old Parkinson’s patient Phil Horton delayed his knee replacement surgery because of past bouts of perioperative delirium where he reported haunting hallucinations and worsening tremors after a prior surgery. Ironically, the medicine used to spare him pain was responsible for his fear. Researchers are more concerned with the levels of anesthesia over the kind given when it comes to causing delirium. Some experts hypothesize that the brain may have trouble reforming the connections between regions that have been “numbed” during anesthesia. Since most anesthetic agents are inhaled, they directly affect the central nervous system and reduce neurotransmitter release at the synapse, which is essential for internal communication. Researchers at Duke University found that general anesthesia renders a patient unconscious by activating the supraoptic nucleus in the hypothalamus to release more of the hormone vasopressin.
These long-lasting fever dreams have begun to raise concerns in elderly patients, especially those with pre-existing conditions. Nearly 200 years have gone by since anesthesia replaced bullet biting, and the exact mechanisms are still unknown. With the rise of alternative therapies, public trust is being stretched as well. The acid trip provoked by psychedelics has been the center of recent clinical trials with the hopes of relieving mental illnesses like depression or post-surgical pain. Incorporating psychedelics into painkiller management will first require much more research surrounding anesthetics.
Image courtesy of Wikimedia Commons