Since the first successful kidney transplant in 1954, human-to-human organ transplantation has remained the best method of treatment for most patients with late-stage organ failure. Although medicine has rapidly advanced since 1954 — including innovations from the insulin pump to CT scans — the fundamental problem of allotransplantation has yet to be resolved: the number of people requiring organ transplants is far greater than the number of organs available.
With roughly 17 people dying each day waiting for a human organ to become available, scientists have responded with a number of novel solutions to the organ shortage. The first major advancement came in 1982, when Dr. William DeVries implanted the Jarvik 7 — the first artificial heart device invented by Dr. Robert Jarvik. Today, engineers and doctors have been able to optimize these devices, enabling patients to live up to five years after transplantation. Though five years may not seem like a long time, artificial hearts are utilized as a bridge for eligible patients on the transplant waitlist or for adding on quality years of life to ineligible patients.
For years, scientists have envisioned a future of 3D-printing or xeno-manufacturing organs.
However, artificial hearts lack the complexity and longevity to adapt to each individual patient, so scientists have turned to regenerative medicine and xenotransplantation — animal-to-human organ transplants. While recently resurging in interest, these ideas are not new. For years, scientists have envisioned a future of 3D-printing or xeno-manufacturing organs. In 1964, James D. Hardy attempted a chimpanzee-to-human heart transplant on a comatose, dying man. Similar attempts have also been made, though patients generally survive only hours to days. The failures of most of the xenotransplants can be attributed to the smaller size of animal organs or to immunological barriers.
Conversely, 3D-printing of organs is still in development but has seen tremendous growth of popularity among biotechnology companies as of late. A race has emerged between 3D-printing organs and xenotransplantation. While 3D-printing can offer autologous organs, it faces a number of challenges in mimicking the complex tissues and muscles of a real organ. On the other hand, animal-to-human transplantation has the benefit of already constructed, non-autologous organs, despite the complex issue of optimizing acceptance by patients. Furthermore, xenotransplantation, rightfully so, has a number of ethical concerns. Questions arise whether or not animals should be used as organ factories for the benefit of human healthcare. Likewise, other than human welfare, the COVID-19 pandemic raises additional concerns with xenotransplantation. The pandemic has driven attention to the risks of zoonotic diseases, bringing along public skepticism for the future of xenotransplantation. However, as studies demonstrate, xenotransplantation poses low risks of passing along viruses such as SARS-CoV-2, HIV, and hepatitis B and C.
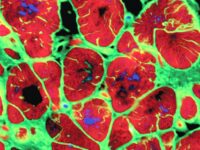
Xenotransplantation can be optimized by two methods: donor species selection and donor species bioengineering. The donor species with the highest likelihood of a successful transplant needs to be identified. While primates are phenotypically the most similar to humans, the size of their organs, risks of infection, and greater ethical concerns limit their likelihood of success. Currently, many scientists believe that swine are the best species to work with, as pigs are easy to breed, have appropriately sized organs, and present lesser ethical barriers. Still, since pigs are so phenotypically different from humans, the xenotransplantation of pig organs is likely to cause rejection in many cases by human patients. As a result, genetic engineering is likely the solution. For example, removing the α1,3-galactosyltransferase enzyme from the swine prevented hyperacute rejections in some pig-to-primate studies.
Though pig-to-human heart transplants are likely years away, a number of companies have recently made breakthroughs in xenotransplantation.
Though pig-to-human heart transplants are likely years away, a number of companies have recently made breakthroughs in xenotransplantation. For example, a Boston-based biotechnology company, Xanotherapeutics, has developed a pig-to-human skin transplant, called Xenoskin. In October of 2019, surgeons at Massachusetts General Hospital in Boston performed a first of its kind xenotransplantation. Surgeons temporarily planted a patch of Xenoskin and a patch of human skin on a burn of a patient. Five days later, surgeons removed both patches and the results were encouraging—both grafts were stuck to the wound bed and were indistinguishable from one another. Though this achievement is very small, it marks a major, successful first step in 21st century xenotransplantation.
Ultimately, both the regenerative medicine and xenotransplantation approaches to organ manufacturing still require much greater study. Though the approaches are vastly different, the primary objective is the same: eliminate the shortage of organs and the dependency on traditional allotransplantation.
Sources:
International Journal of Surgery (2015). DOI: https://doi.org/10.1016/j.ijsu.2014.12.011