For nearly 1.7 million Americans affected by type 1 diabetes, the thought of being free from a lifetime of insulin therapy is unheard of. However, a recipient of a new stem cell–based therapy is producing her own insulin less than three months after the injections.
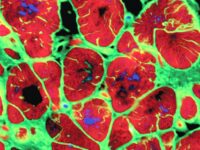
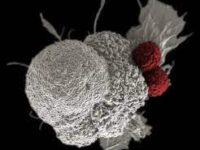
Type 1 diabetes (T1D) is an autoimmune disorder that destroys islet cells, the cells in the pancreas that naturally produce insulin. Insulin is required for glucose to enter cells and be metabolized into energy. With insufficient levels of insulin, patients experience constant thirst, frequent urination, weight loss, and chronic tiredness. The cause of type 1 diabetes is relatively unknown, which makes preventative therapies difficult. Current treatment involves lifetime insulin supply therapy, typically consisting of roughly three daily insulin injections or an insulin pump. Despite daily management, complications of type 1 diabetes are still of concern. High levels of glucose can lead to heart disease, foot and blood circulation problems, vision complications and blindness, nerve damage, and kidney disease. These complications would require further more intense treatment.
“A recipient of a new stem cell-based therapy is producing her own insulin less than three months after the injections.”
Since type 1 diabetes destroys islet cells, transplantation may be a valid therapeutic pathway. However, there aren’t enough donors to meet the demand for islet cell transplants. This is where stem cell technology comes in. Stem cells are undifferentiated cells, meaning they have the potential to develop into any type of cell based on genetic direction. Induced pluripotent stem cells (IPSCs) are generic blood or skin-derived cells that can be reprogrammed back into their embryonic–like, undifferentiated state. The stem cell’s ability to become any type of tissue cell is known as pluripotency and enables researchers to utilize an unlimited supply of any type of human cell.
Hongkui Deng PhD, a cell biologist at Peking University in Beijing China, is the lead researcher of a study published in Cell. With a background in induced pluripotent stem cell development, Deng’s team discovered a method to create and implant insulin–producing cells.
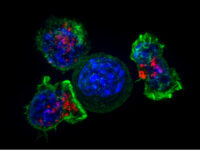
Deng’s team at Peking University focused on a singular patient case: a woman from Tianjin, China who had undergone two liver transplants and a failed pancreas transplant. For this woman, insulin supply therapy was not sufficient, making her a good candidate for the trial. Deng and his colleagues extracted fat tissue from the patient and reprogrammed them to induce pluripotency. The IPSCs were then programmed to produce insulin–like natural islet cells. In a procedure of less than half an hour, Deng’s team injected around 1500 stem cell derived islet cells into the patient’s abdominal muscles. By injecting the cells into the abdominal muscles instead of directly into the liver, the team would be able to monitor the cells via imaging and remove them if needed.
Just after two and a half months, the recipient of the therapy was producing a sufficient amount of insulin without any supplemental therapy and has since sustained this for over a year. Her blood glucose levels are within the target range for 98% of the day. The results are “remarkable,” according to researchers like Daisuke Yabe at Kyoto University, who has high hopes for application in other diabetic patients. More trials and studies will be needed to corroborate the results of Deng’s team and commercialize this process, researchers say.
Similar therapies for T1D are being developed in the pharmaceutical world. For example, Vertex Pharmaceuticals, located in Boston, MA, currently has two ongoing clinical trials of drugs VX-880 and VX-264 that consist of fully differentiated islet cells. However, it should be noted that if a patient’s own cells are not being used to develop the IPSCs, such as with Vertex’s drugs, the therapy must be given in conjunction with immunosuppressive therapy. Immunosuppressive therapy is necessary to reduce the immune response and prevent rejection of the foreign cells and drug therapy.
While the therapy still has a long way to go, IPSC therapy may allow for the treatment of various autoimmune diseases and provide hope to the large population of patients with chronic diseases.
“IPSC therapy may allow for the treatment of various autoimmune diseases and provide hope to the large population of patients with chronic diseases.”