By May 2022, over 1 million people had died due to COVID-19 in the United States. The COVID-19 illness, which refers to the set of symptoms people experience, is caused by the acute respiratory syndrome coronavirus-2 (SARS-CoV-2) virus. The pandemic has not only affected the United States but the entire world as well. This respiratory virus has resulted in 5.5 million deaths out of the 272 million cases reported worldwide up through December 2021.
Though it seems that the pandemic has subsided as politicians push to return back to “normal,” many are still trying to seek preventative measures to protect themselves against serious illness. One of these preventative measures created in efforts to get those less receptive to vaccination is the Paxlovid pills. For those who are weary of the vaccine or unable to receive it due to other health reasons but still want a way to combat the illness, the pills can act as a solution to individuals who contract the virus.
However, it is important to note that the pills do not act as a replacement for the vaccines, for vaccines are injected into one’s body when a person does not have the virus yet and helps reduce the symptoms of the illness and chance of death if one were to contract it. Rather, the pills can act as a less invasive treatment when one has symptoms and it is too late to consider the vaccine as an option. So for those who may not be able to receive the vaccine or chose not to, they have another option to help reduce the symptoms of the virus.
The pills can act as a less invasive treatment when one has symptoms and it is too late to consider the vaccine as an option.
Though the drug was granted usage by the U.S Drug and Food Administration back in December 2021, many citizens are still unaware of the drug and its effects and benefits. The prescription of the drug by doctors and medical professionals have gone down, with many patients unaware that there is a medication that may help them combat their symptoms of COVID-19. As Paxlovid sits on shelves of pharmacies fully instock, the virus’s cases and deaths still rise, showing the public health failure in communicating the benefits of taking Paxlovid.
So what is Paxlovid?
“It is the beginning of a ‘game-changer,’” said Dr. Scott Roverts, a Yale medicine infectious disease specialist.
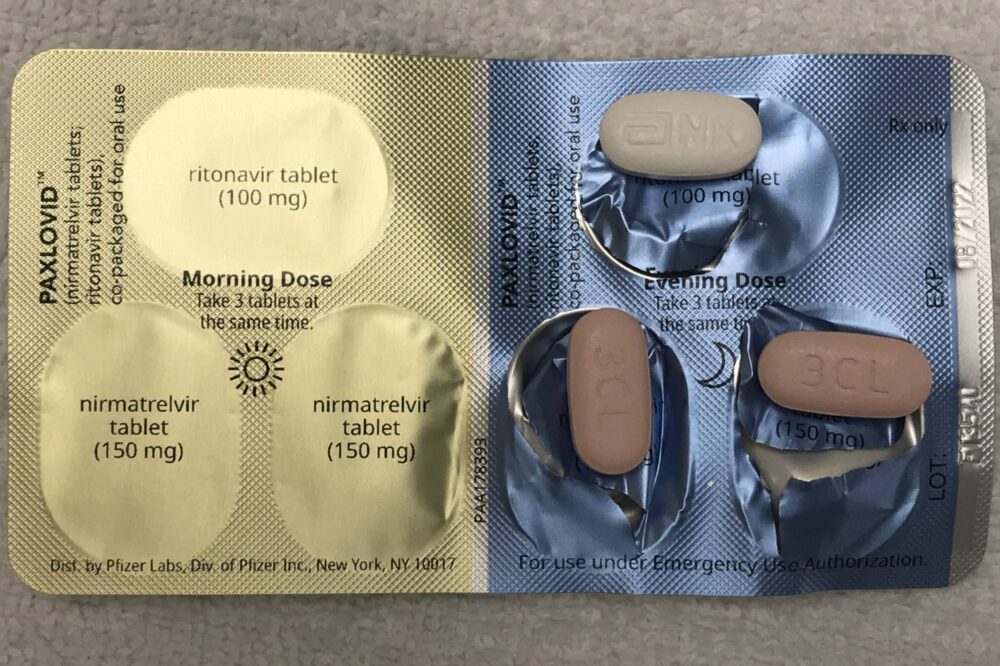
If one were to take the pill, the individual would need to take up to three Paxlovid pills twice a day for over five consecutive days, taking a total of 30 pills. Thus, patients should consider, based on scientific studies, the efficiency of the treatment administered through oral pills after testing positive for the virus.
In order to understand how the drug works, there needs to be an understanding of how the virus works. There have been many variants of the virus, including alpha, beta, delta, gamma, and omicron. SARS-CoV-2, which is where all these variations stem from, is made up of four structural proteins: spike glycoproteins (S), small envelope glycoproteins (E), glycoproteins membrane (M), and nucleocapsids (N).
The spike protein allows the virus to enter the cell. Then, once inside, the virus hijacks the cell’s DNA replication mechanism to replicate itself. The spike proteins are the foundation for where vaccine development targets. Along with the four main structural proteins, the SARS-CoV-2’s genome also includes two polyproteins known as Pp1a and Pp1ab. These polyproteins are important because they act as markers telling the Mpro protease where to cut the different proteins in the virus to create more manageable and non-tangled chunks for replication. Along with targeting the spike protein, inhibiting SARS-Cov-2 Mpro has become the main concentration for antiviral therapy such as Paxlovid.
If one were to take the pill, the individual would need to take up to three Paxlovid pills twice a day for over five consecutive days, taking a total of 30 pills.
Paxlovid, the brand name of the drug, is composed of nirmatrelvir and ritonavir. These two were among other drugs that were in clinical trials, and it was found that the combination of nirmatrelvir and ritonavir provides the most effective results, giving an 89% reduction in the risk of death. Nirmatrelvir was created from a Pfizer research program in 2002 and was investigated on how it combated the SARS family of viruses by targeting the Mpro protease. One limitation with nirmatrelvir is that the drug could only be administered by direct injection into a vein. So in 2020, Pfizer worked on how to make this drug effective orally.
Ritonavir also works as a protease inhibitor, but did not start out as a way to combat SARS. When ritonavir and nirmatrelvir are combined to form Paxlovid, they act together, with the added benefit of ritonavir inhibiting the breakdown of the nirmatrelvir in the liver. This enables a higher drug concentration and helps it to be more effective at fighting against SARS for a longer time.
Many COVID-19 patients who received Paxlovid report significant improvements in symptoms. However, some experienced a second worsening of symptoms in the following weeks. This is not due to the lack of effectiveness of the pill, but rather the drug fulfilling its’ responsibilities of being a short term solution to relieve severe viral symptoms.
BMJ (2022). DOI: 10.1136/bmj.o926
BMJ (2022). DOI: 10.1136/bmj.o1037
Antibiotics (2022). DOI: 10.3390/antibiotics11020220