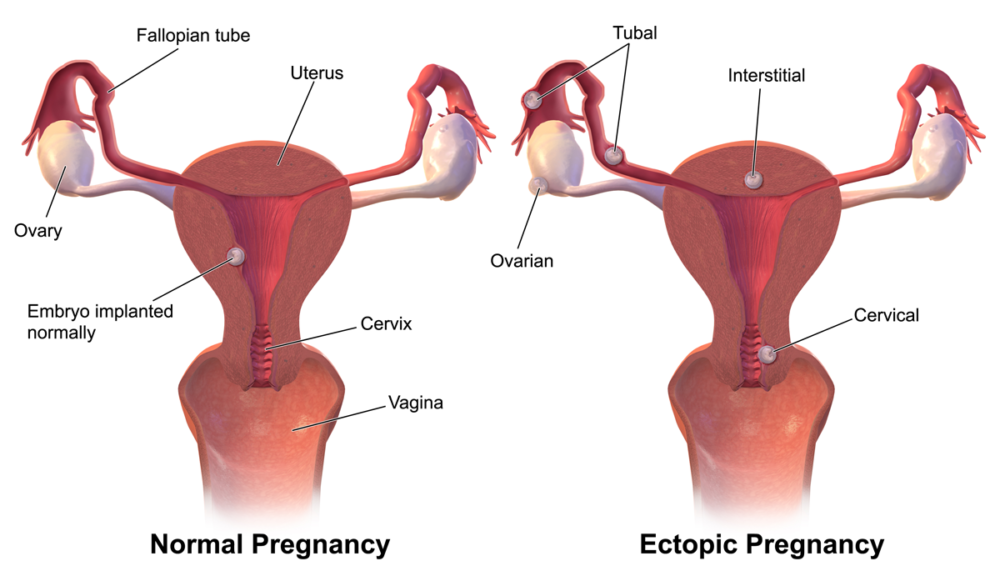
Pregnancy is an uncertain time for many expectant parents. It’s a daunting experience known for its vast expanse of new territory and potentially risky outcomes. A constant in most pregnancies is the location of the embryo: in the protective, developmentally beneficial environment of the uterus. However, this isn’t always the case. The prevalence of extrauterine implantation is rising, resulting in increased awareness surrounding bilateral ectopic and heterotopic pregnancies. For ectopic pregnancies, embryos are implanted within both fallopian tubes, while extrauterine pregnancies are present simultaneously with an intrauterine embryo. Both instances are extremely rare when the fetus is conceived without fertility treatment, but the use of reproductive assistive technology and prevalence of ectopic implantations appear to be associated, revealing a serious concern for those who fail to receive accurate and timely diagnoses of these conditions.
A constant in most pregnancies is the location of the embryo: in the protective, developmentally beneficial environment of the uterus. However, this isn’t always the case.
A 2014 case study from the Women’s Hospital at Zhejiang University School of Medicine investigated a bilateral ectopic pregnancy that occurred in a patient who conceived on her third round of ovulation induction. Fifteen days after the patient’s insemination, she was admitted to the hospital due to some vaginal bleeding. Tests were ordered for beta-human chorionic gonadotropin (β-hCG), a hormone present in the urine and blood of pregnant individuals. The results revealed levels of β-hCG consistent with being two to three weeks pregnant. However, eight days following her first hospital visit, the patient was admitted to the emergency room with severe pain in her lower right abdomen and a β-hCG level typical for someone five to six weeks pregnant. Transvaginal ultrasonography revealed a mass within the region of her right fallopian tube and a salpingectomy — or fallopian tube removal — was performed. After being released from the hospital, the patient’s β-hCG levels began to increase again and a second mass was discovered 21 days after the initial surgery, leading to the discovery of a second ectopic pregnancy in her left fallopian tube and another salpingectomy. The atypical development and diagnostic difficulty further emphasize the importance of consistent caution throughout early pregnancy due to the possibility of ectopic development.
Eight days following her first hospital visit, the patient was admitted to the emergency room with severe pain in her lower right abdomen and a β-hCG level typical for someone five to six weeks pregnant.
Meanwhile, another case in 2012 from the Institute of Gynecology and Obstetrics at the Clinic Center of Serbia details an instance of abnormal embryo implantation through in vitro fertilization. In their first trimester of pregnancy, a patient was admitted to the hospital for severe abdomen pain. Despite her pain, an ultrasound of the abdominal region showed typical placement of her organs consistent with the growth of the viable pregnancy located in her uterus. Continued observation revealed tenderness in her lower abdomen, but further transabdominal scans showed typical fetal development and the cause of the pain remained undiagnosed. Two hours after receiving intravenous fluids and a blood transfusion to improve her blood pressure, the patient displayed signs of hemorrhagic shock and her blood pressure had decreased dangerously. Despite the patient’s medical record detailing previous ectopic implantation, it was only at this point that the possibility of ectopic pregnancy was first considered. A senior obstetrician was consulted to perform a transvaginal ultrasound and found a mass attributed to an ectopic pregnancy. The pregnancy had ruptured, necessitating an immediate removal of the right fallopian tube and termination of the intrauterine pregnancy.
Ultimately, the patient recovered, but doctors and data suggest that the use of multiple embryos during in vitro fertilization treatment contributes to a higher risk of ectopic pregnancies. Typically, heterotopic pregnancies are not discovered until after the ectopic implantation has ruptured, often resulting in the patient requiring significant medical care to resolve potentially fatal hypovolemic shock, deeming the heart unable to pump blood throughout the body.
Doctors and data suggest that the use of multiple embryos during in vitro fertilization treatment contributes to a higher risk of ectopic pregnancies.
Within both case studies, development issues within the patients’ pregnancies were left undetected until the symptoms became so severe that surgery and permanent consequences resulted. Not only do bilateral ectopic and heterotopic pregnancies frequently result in dismissal or minimization of the patient’s symptoms, but they can also be potentially fatal in the instance of ectopic ruptures. To ensure the safety and health of pregnant individuals, particularly those using assistive reproductive technology, healthcare providers must be attentive to the possibility of the diagnosis of these dangerous “hidden” pregnancies.
Journal of Zhejiang University-SCIENCE B (2014). DOI: 10.1631/jzus.B1400081
Srp Arh Celok Lek (2012). DOI: 10.2298/SARH1208511S