With Northeastern University having recently climbed the academic ladder to become a tier one research institution, hundreds of projects are simultaneously emerging with the aim of publishing innovative information. In a newly published study, Northeastern Research Associate Professor Christine Lary collaborated with the Division Chief of Pediatric Oncology at the Tufts University School of Medicine, Dr. Aaron Weiss. Using Lary’s knowledge in biostatistics and Weiss’s clinical experience, they explored the use of an immunosuppressive drug called sirolimus on patients with desmoid-type fibromatosis.
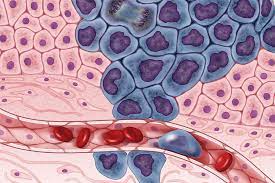
Primarily affecting young adults and children, desmoid tumors are soft-tissue, non-cancerous growths with a high incidence of local-recurrence and aggression. This means that the mass often grows back after removal in the same spot, or very close to its original spot. Due to the tumor’s aggressive nature and specific demographic, the pair directed their research to discover if the drug sirolimus could be used to block the mTOR signaling pathway that is often associated with tumors. mTOR plays an essential role in tumor metabolism as it leads to gene transcription and protein synthesis, both of which are essential processes for cell growth and tumor expansion. More cells means more tumor cells, which is why Dr. Weiss aimed to discover how to block a pathway responsible for cell expansion. Sirolimus was selected as the drug of interest due to its relatively low cost and ability to be administered orally. Typically used to suppress the immune system after a transplant surgery and prevent the rejection of a new organ, the drug also targets the mTOR pathway.
The study consisted of nine subjects under the age of thirty with desmoid tumors at a low risk of recurrence, which is determined by factors such as size and anatomical location. The participants took sirolimus orally for three days before surgical removal of the tumors. Over four weeks, the researchers observed the patients for instances of recurrence and noted their reported levels of discomfort to test if the drug helped to improve any pain derived from the tumor.
After tumor removal, the data indicated that the drug had no noticeable influence on pain, and the reported levels of proteins involved with the mTOR pathway had conflicting results. It was discovered that there was an increase in one downstream protein (p4EBP) and a decrease in the other (pS706k). Theoretically, both should have decreased due to their functions in the pathway, so the observed levels were a little confusing.
“It’s hard to gauge the exact reason why one protein decreased and not the other,” Dr. Weiss said. “When you do these types of studies, you never know what you’re going to find. If we could have adjusted the doses during the study and got certain patients to higher levels, maybe we would have seen an impact on the proteins.”
“‘When you do these types of studies, you never know what you’re going to find,’ said Dr. Weiss.”
Dr. Weiss hypothesizes that both the drug’s dosage and duration of administration may have been significantly too low. Additionally, he acknowledged that the sample size for the trial was smaller than originally anticipated, given that the modern field of oncology is generally moving away from surgical resection if possible. This is because the risks of surgery, including infection or other complications, may not outweigh the potential benefits. In oncology, a tumor has to be completely removed with no leftover mass to ensure no regrowth. For this reason, treatments such as chemotherapy or other targeted therapies are occasionally preferred. Moreover, some tumors, including desmoid tumors, are known to sometimes spontaneously regress or shrink in size. The reasons behind spontaneous regression are not entirely clear, but it is clear that most surgeons would rather observe their patient than perform an operation when possible. As this trial was initially structured back in 2011, Dr. Weiss could not have foreseen this shift in general practice.
“In an ideal world, I would love to be able to still answer the question of whether sirolimus — or a drug that impacts this pathway — would be beneficial for patients with desmoid tumors,” said Dr. Weiss. “You need a lot of money in order to do a real study, and that’s hard to get.”
Overall, the researchers acknowledged the study as exploratory research, and they established that the drug could be safely administered to children and young adults: their target demographic. Although Lary and Dr. Weiss may not have been able to reach any definitive conclusions, they established the groundwork for future research into sirolimus and the mTOR signaling pathway. If sirolimus is discovered to impact the pathway, thousands of non-desmoid-tumor patients could benefit as well, since mTOR has been connected to breast, lung, prostate, gastric, lymphoma, urinary, neck, and many other cancers.
Applying for research funding is notoriously competitive and time-consuming. So, “if you’re gonna make advances in the field, you’re going to have to collaborate,” said Dr. Weiss. After all, research is a collaborative effort. The intent of research is to better the scientific community’s collective knowledge; each study is simply a piece of the puzzle.