Beginning signs of dementia and Alzheimer’s disease can start up to 18 years before a diagnosis ever occurs. In the almost two decades it takes to receive a diagnosis, so much damage has already taken place in the brain that treatment measures can only alleviate symptoms and extend life expectancy by a few years. But, if a diagnosis were to occur earlier in the disease’s progression, could we extend this expectancy further or increase the chance of finding a true cure at last?
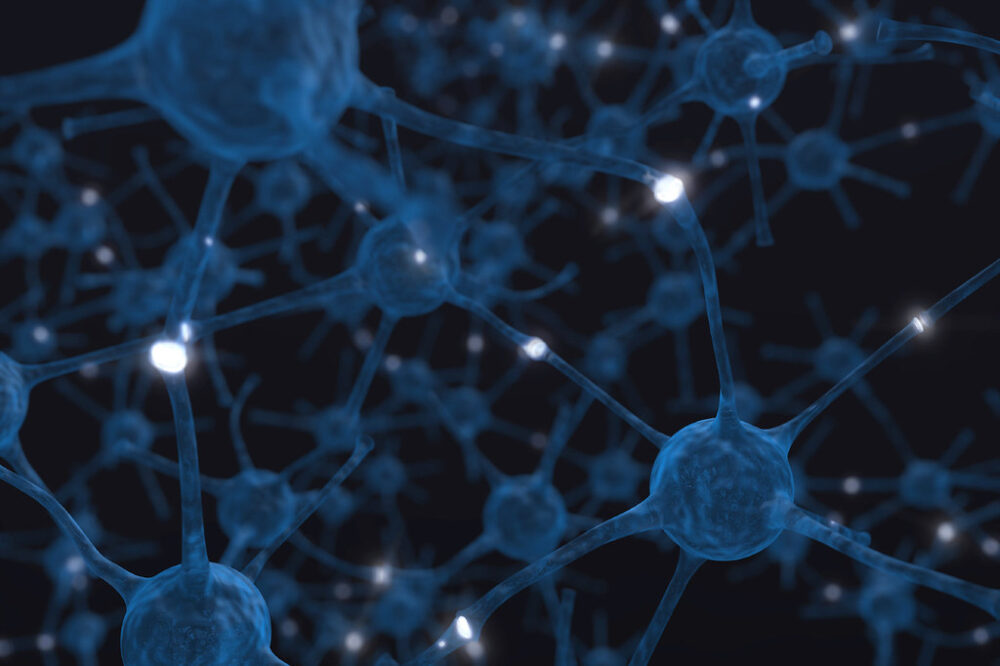
“Neurons underlie neurological diseases, and they rely on fractal geometry for their connectivity and function.”
Neurons underlie neurological diseases, and they rely on fractal geometry for their connectivity and function. Dendrites are the communication hubs of neurons and have a branch-like form that allows for optimal information transfer. Consequently, they are an integral player in brain function. Used similarly in lightning, rivers, and trees, this fractal branch pattern is used specifically by dendrites to extend their reach as well as increase the surface area for incoming synapses, the actual site of message transmission. All in all, this geometric pattern allows for more efficient communication between neurons in the brain.
Over time, new technology has emerged that allows for earlier diagnosis of Alzheimer’s disease. More recently, certain positron emission tomography (PET) tracers have been able to show amyloid buildup and increased amounts of tau protein. In normal circumstances, amyloid is essential for neuron growth and repair, but in Alzheimer’s, abnormal levels of the protein build up into plaques which disrupt critical neuronal function. Tau protein is responsible for maintaining neuronal signaling and structure, but its dysfunctional state causes neurofibrillary tangles. As hallmarks of Alzheimer’s, both amyloid plaques and tau cause a decrease in neuron signaling and massive neurodegeneration, eventually leading to brain atrophy. This consequently translates into traditional Alzheimer’s symptoms related to impaired memory, thinking, and execution of everyday activities.
While PET scans can detect unusual cellular activity, like amyloid plaques and increased tau presence, they are not commonly performed. Instead, magnetic resonance imaging (MRI) scans are heavily favored and already prevalent within medicine and research. MRI scans do not provide the same insights as PET scans but instead offer very high spatial resolution. Within our understanding and interpretations of MRI scans, a new metric called fractal dimension is emerging as a forward method for early diagnosis of neurodegenerative diseases such as Alzheimer’s. Fractal dimension is a numerical representation of the structural complexity between neurons’ communication points and also gives a more quantifiable understanding of the signaling occurring.
It has long been understood that fractal dimension decreases with age alongside other factors like gender, but in his 2014 study, Richard D. King, a professor from the University of Utah, showed that diseases like Alzheimer’s can also influence fractal dimension values. He found that when compared to a healthy adult, those with Alzheimer’s have lower local fractal values in the brain’s cortex. Additionally, a study by Ryuta Kinno and his team at Showa University School of Medicine found a significant correlation between the metric and memory evaluation techniques like subject recognition and paired associate memory abilities. The lower fractal values reveal a decrease in neural communications and indicate that the signals being sent are less efficient. This again supports the idea that a decrease in fractal dimension could be indicative of Alzheimer’s disease.
By continuing to study and one day incorporating this fractal dimension into everyday diagnostics, perhaps we will be one step closer to finding a true cure for this harrowing disease.