Modern medical advancements are largely dependent upon the strength of the technology used in the field. The skills of surgeons are enhanced by sophisticated tools that can be used in and out of the operating room. A recent, notable advancement in medical technology is the increased use of the intraoperative magnetic resonance imaging (iMRI) exam, which monitors real-time changes of a patient during an operation.
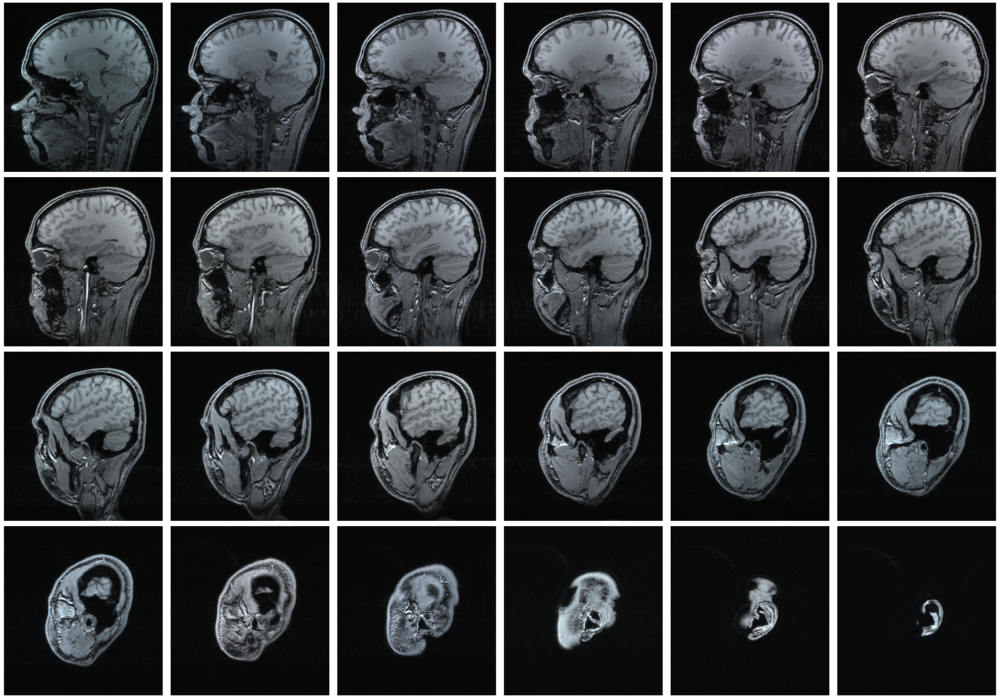
As described in a plain language review by Abi Berger, an MRI is commonly composed of very strong magnets which create a magnetic field. This magnetic field aligns protons throughout the area of interest. Oftentimes, the protons of hydrogen atoms are targeted by this machine due to their ubiquity in various body tissues. The strong magnetic field created by the MRI machine forces the poles of the hydrogen protons to align. Once the protons are aligned, radio waves are sent through the machine. This radio frequency offsets the magnetic field. When the machine-produced radio waves are turned off, the magnetic field reverts to its normal position, which emits radio waves. These waves are used to produce the image for the MRI.
The signal from these re-emitted radio waves can be detected by coils placed throughout the machine. Various body parts and tissues can be identified by comparing the time it takes for the magnetic field to return to its normal state (T1 relaxation) and the time it takes for the spin of atoms to revert to their normal position (T2 relaxation). By documenting the various T1 and T2 times, disease and irregularities in pathology can be identified.
Oftentimes, MRIs are used as a diagnostic tool. However, the development of the intraoperative MRI has enabled this tool to be used throughout the patient’s case. The development of the iMRI has various applications, many of which pertaining to brain imaging and neurosurgery.
The iMRI allows for the monitoring of the “brain shift phenomenon.” This occurs due to the changing cranial anatomy upon various operating conditions. For example, the addition of anesthetics, ventilation techniques, and the exposure of the brain to the atmosphere forces changes in the brain that may not align with what was seen in the preoperative scans.
Neurosurgeons are also able to determine their tumor resection margins throughout the surgery. MRIs are commonly used for preoperative information, so using the same method of information gathering pre-surgery and during surgery is an incredible resource because the surgeons are able to perfectly compare the before and after images.
Despite the incredible implications of the iMRI, it is not quite ubiquitous yet due to the incredible cost and effort it takes into creating a space for an iMRI. In order to adopt the technology, the hospital or place of operation should strive to allow uninterrupted patient access during the iMRI. Oftentimes, this entails creating a special iMRI operating space. A major portion of this necessity is for anesthesiologists to be able to maintain proper ventilation and monitoring for the patient. Therefore, the equipment used by anesthesiologists must be compatible with an iMRI suite. The equipment must be non-ferrous, meaning the metal used does not contain iron.
The areas in which the iMRI will be used must be free of any magnetic field in order for the machine to operate properly and avoid any damages to surgical equipment or the machine. This forces the establishment of zones within the iMRI operating space as well as the use of compatible equipment.
The various spatial and material requirements for an iMRI operating field have spawned the practice of a dual operating room. This separates the operating suites into the main corridor and the iMRI room that can be used when the surgeon deems it necessary.
The iMRI is an incredibly useful technology in terms of enabling real-time surgical updates; however, the cost and incredible care it takes to operate an iMRI make this revolutionary practice difficult to implement.
Sources:
Indian Journal of Anaesthesia (2018). DOI: 10.4103/ija.IJA_29_18
BMJ (2002). DOI: 10.1136/bmj.324.7328.35
Journal of Neuro-Oncology (2021). DOI: 10.1007/s11060-020-03667-6