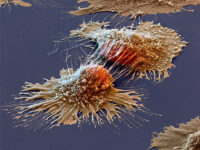
Studies show that anywhere from 30% to 50% of the tumor mass in glioblastoma, an aggressive brain cancer, is actually made of our own immune cells. Glioblastoma is an elusive and dangerous tumor type. Only a quarter of patients live longer than a year, and less than 10% survive longer than five years. It grows remarkably quickly, and there is no clear cause for this rapid development. It’s also quite difficult for our bodies to defend against. This is because the tumor’s cellular and cardiovascular surroundings, called the tumor microenvironment, functionally suppresses the body’s T-cells. T-cells are a type of immune cell that would typically target and kill glioblastoma cells. With the immune system’s first line of defense gone, glioblastoma are able to wreak havoc from the inside.
A 2024 study headed by Daan Kloosterman determined that glioblastoma cells recruit a particular subtype of macrophages to collect lipids that help them grow, fueling tumor progression and aiding immunosuppression of T-cells. The involvement of these “lipid-laden macrophages,” or LLMs, is associated with an even poorer prognosis in patients with glioblastoma. Given that most current macrophage-targeted therapies aren’t very effective, Kloosterman’s study proposed a few ideas as to how the hijacking of macrophages can be prevented, with the reminder that there is still much to learn and explore about these tumors.
“Glioblastoma cells recruit a particular subtype of macrophages to collect lipids that help them grow, fueling tumor progression and aiding immunosuppression of T-cells.”
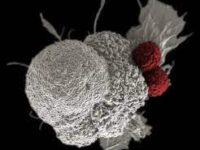
Macrophages normally play two key roles in our immune systems. First, they are phagocytes, meaning they digest dead cells, bacteria, debris, and even tumor cells. Second, macrophages can be crucial in enhancing the body’s adaptive immune response. Unlike the innate immune response, which sparks inflammation and utilizes various proteins and enzymes for rapid defense, the adaptive immune response takes effect later and uses more specialized cells for direct attacks. Macrophages in the adaptive immune response can present antigens to T-cells or initiate lymphoid cell-mediated tumor resistance mechanisms. In simple terms, macrophages make it difficult for tumors to grow and for cancer to spread.
There are several different subtypes of macrophages, one of which has been associated with more aggressive cases of glioblastoma. Lipid-laden macrophages (LLMs) are cells that accumulate surrounding lipids and alter lipid metabolism in order to adapt to challenges. Kloosterman’s team used molecular analyses on glioblastoma cells and found that LLMs tend to accumulate in hypoxic (oxygen-deprived) areas, which is also where glioblastoma thrives. They then ran a series of other experiments to explore the exact relationship between LLMs and glioblastoma.
One of the major findings of the study was that glioblastoma uses some genetic properties of LLMs to eliminate the threat of T-cells. LLMs accumulating in hypoxic spots were found to have reduced chromatin availability in inflammatory genes. Since inflammation is a key step in the immune response, the change in chromatin availability ultimately results in increased immunosuppression. Additionally, it jeopardizes antigen presentation, meaning T-cells are unable to function.
Kloosterman’s lab also concluded that glioblastoma cells instruct LLMs to deliver nutrients that help it grow and proliferate. A lipid analysis of accumulated LLMs showed that the lipids in the tumor microenvironment were from external sources; they weren’t newly synthesized by the glioblastoma or macrophages in the microenvironment. This suggests that LLMs collect lipid debris from nearby myelin that wraps around neurons in the brain. Lipid accumulation benefits the glioblastoma cells because they naturally have low lipid content, so they rely on the LLMs’ scavenged myelin to fuel its proliferation.
Although studies like this one clearly show that macrophages could be excellent targets in cancer therapy, many current developments are incompatible with the cells’ defense mechanisms, leading to adverse reactions. For this reason, Kloosterman’s team tested a few new ideas that interfere with glioblastoma commandeering LLMs. One such idea was to inhibit the protein CD36 using a solution called sulfosuccinimidyl oleate, or SSO. This successfully prevented myelin uptake in LLMs. Additionally, when they inhibited the lipid-export protein ABCA1, this was able to block the transfer of lipids to glioblastoma. They also treated mice who had been infected by glioblastoma with SSO, which increased survival rates. Finally, the researchers treated glioblastoma cells with SSO or with inhibitors of ACA1 or LXR in vitro, and this limited the pro-proliferative effects of LLMs.
While these results are encouraging, it’s important to remember that cancer therapies are less often one size fits all, and scientists and clinicians may need to create and utilize combinations of treatments that not only terminate the macrophage’s role in immunosuppression, but also reactivate T-cells. The primary treatment plan for glioblastoma currently includes chemotherapy, radiotherapy, and surgery. As shown by glioblastoma’s dismal prognosis, these treatments are largely ineffective. Researchers are exploring numerous approaches to targeting or utilizing tumor-associated macrophages in therapies. Some of these include reducing the number of LLMs, reprogramming LLMs from a pro-tumoral phenotype to an anti-tumoral phenotype, enhancing phagocytosis of tumor cells, and decreasing glioblastoma’s recruitment of LLMs.
Furthermore, combination therapies may prove beneficial for other types of tumors known for high immunosuppression. Preclinical studies have tried inhibiting proteins involved with tumor-promoting bone marrow cells. Another strategy is to target proteins involved with immune checkpoints. Others found potential in the development of chimeric antigen receptor effector (CAR-T) cells. CAR-T cells are genetically engineered T-cells that are designed to recognize, bind to, and kill certain cancer cells. Research indicates that, with further exploration and fine-tuning, various combination therapies could be used to treat not only glioblastoma but also cervical, lung, and ovarian cancers, in addition to multiple types of sarcomas. The development of effective macrophage-targeted cancer therapies is certainly a milestone that researchers are striving for, especially those that inhibit proteins and interfere with cellular checkpoints. Such studies illustrate the exciting reality that there’s much to be uncovered about the interaction between cancer and the immune system.