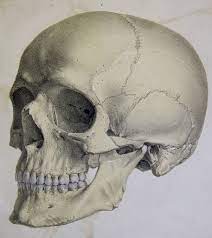
Tucker Marr, an avid hockey player and analyst at Deloitte, suffered a fractured right skull and a subdural hematoma after falling down a flight of stairs. These injuries are critical and warrant emergency surgical treatment, a procedure called a craniectomy.
Craniotomies are performed to reduce swelling, pressure, or bleeding in the brain, all of which are extremely dangerous and may cause severe brain damage. In this emergency surgery, causes are usually drastic and happen promptly after a traumatic injury, stroke, clot, or hematoma. The procedure usually goes as follows: the patient must shave their head near the incision site, the surgeon will make the incision and expose the skull, the surgeon will then remove a piece of the skull, treat the reason for the craniectomy, cover the brain with a mesh material, and finally close the incision. However, this leaves patients with a visible malformation of the skull and the brain exposed directly under the skin. In the future, patients are able to go back and possibly have the malformation corrected with a piece of skull bone placed back into the head, a risky and costly procedure called a cranioplasty.
After the surgery, Marr put his active lifestyle on hold and was required to wear a helmet for protection and to keep the indentation on his head hidden. As the days went on, Marr lacked confidence and felt dizzy and fatigued, as his brain was unshielded from atmospheric pressure. Marr and his family knew that they needed to explore other options.
After researching the tried-and-true skull replacement surgery, Marr discovered that this surgery had a high rate of infection and would be costly in the long run because of monitoring procedures such as MRI or additional surgeries to see into the brain. Marr took initiative and investigated a cutting-edge surgery that utilized modern additive manufacturing: instead of placing the skull bone fragment back, it would be replaced with a different prosthetic fragment. He presented a procedure that was still in the early phases of research, using a 3D printer to manufacture an acrylic prosthetic skull fragment to replace the part of his skull that had been removed. Dr. Netanel Ben-Shalom, a neurosurgeon and assistant professor of neurology, took notice of Marr’s request, resulting in a collaboration to create this patient-specific implant to replace the resected area of the skull.
Using an acrylic material to replace the bone offers a notable advantage to medical professionals – now, only an ultrasound is needed to look at the patient’s brain. This idea is dubbed “acrylic windows” since the clear material offers a quicker and minimally invasive way to assess a patient’s brain post-operation. Currently, very few medical centers offer acrylic windows for patients since the procedure is still in the initial stages of research.
Marr eventually received the surgery he wished for, and after the acrylic prosthetic was implanted, he felt more confident, regained his physical abilities, and reported that his symptoms from the exposed brain had dissipated. Now, working with Dr. Ben-Shalom, Marr is able to have easy check-ups and teaches medical students about this state-of-the-art technique.
However, new advancements in the medical field are often met with both support and resistance. Favors of this technique argue that this development is extremely valuable – especially since patients with craniotomies often require long-term monitoring and regular brain imaging. By using acrylic windows, medical professionals can easily assess the physiological causes of symptoms by using an ultrasound rather than other expensive and limited methods such as CT and MRI scans (which often require resources and analysis from other departments, such as radiology). On the other hand, other medical professionals believe that further evidence is needed to confirm that ultrasounds are equally as accurate as higher-order scans. Due to the early stages of this research technology, some medical professionals are still wary of the ability of ultrasounds to match the imaging details seen in higher-order scans.
“Using an acrylic material to replace the bone offers a notable advantage to medical professionals – now, only an ultrasound is needed to look at the patient’s brain. “
Dr. Ben-Shalom told the New York Times that, in his experience, as long as the acrylic window is placed in the correct spot, the cavity of interest would be clearly demonstrated. Looking into Marr’s brain at his regular checkups, Dr. Ben-Shalom can see how the midline of the brain that separates the two hemispheres looks (as this was pushed to the side after his initial craniectomy), the structures of his brain, and even the pulsing of his brain. If Marr were to ever have symptoms that would warrant Dr. Ben-Shalom to look into his brain, it would be done quickly and with ease. Dr. Ben-Shalom continues to specialize in this reconstructive surgery, and offer more patients who have undergone craniotomies the chance to look and feel like themselves again.