We are often reminded of basic health mantras to decrease your risk of getting cancer such as wearing sunscreen, avoiding smoking, and being wary of carcinogens. It might surprise you to hear that increasing your caffeine intake might be added to the list.
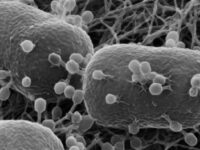
The concepts for this idea emerged in the early 2000s, when Michail Sitkovsky, director of Northeastern’s New England Inflammation and Tissue Protection Institute, discovered that a specific receptor, the A2A adenosine receptor, inhibits immune cells from invading tumors. This enables the growth, proliferation, and spread of the tumor. It has long been known that tumor cells rapidly exhaust their blood supply, creating a low-oxygen environment. This oxygen shortage encourages the production of adenosine, which reacts with the A2A adenosine receptor to put local tumor-fighting immune cells to sleep. For years, researchers sought a drug that could combat this adenosine effect, but, Sitkovsky wondered, what if the solution was more simple than it seemed?
This question encouraged him to address the root of the issue: oxygen access. He and his colleagues found that access to supplemental oxygen — supplying the blood with two to three times more oxygen than typical — helps mitigate this A2A signaling and encourages immune cells to invade the tumor. These increased oxygen levels, known as “respiratory hyperoxia,” were also found to stifle the spread of breast tumors. This mechanism serves as a potential avenue for enhancing the power of immunotherapies, a treatment method in which the body’s own immune system is stimulated to specifically target cancer cells.
“Breathing supplemental oxygen opens up the gates of the tumor fortress and wakes up ‘sleepy’ antitumor cells, enabling these soldiers to enter the fortress and destroy it,” Sitkovsky said. “However, if antitumor immune cells are not present, oxygen will have no impact.”
Although respiratory hyperoxia is a powerful tool to equip the immune system, Sitkovsky hypothesized that more could be done to further inhibit the A2A receptor. For years, epidemiologists had found a link between coffee consumption and decreased cancer risk. Indeed, research from him and his colleagues in 2009 found that caffeine, a natural antagonist of the A2A adenosine receptor, further enhances the therapeutic impact of respiratory hyperoxia.
‘This mechanism has the unique capability to not only be effective on its own, but boost the efficacy of other targeted therapies of cancer,’ Sitkosky said.”
“Many of us consume coffee every day to keep ourselves awake and functional during the day. Our addiction might be helping us out in the long run!” Sitkovsky said.
Although some years have passed since this groundbreaking discovery, this mechanism has expanded beyond the original idea of cancer therapy. More recently, Sitkovsky points to the A2A receptor’s role in treating patients with COVID-19-triggered pneumonia. Sitkovsky recalls how in the early months of 2020, COVID-19 was tearing through Italy’s elderly population. This time, he worked with clinicians in Italy to explore the impact of administering adenosine to prevent inflammatory damage to the lungs. Although the study was small, it found that the presence of COVID-19 RNA rapidly decreased in 13 out of 14 cases within seven days, compared to no changes in the control group.
“‘Breathing supplemental oxygen opens up the gates of the tumor fortress and wakes up ‘sleepy’ antitumor cells, enabling these soldiers to enter the fortress and destroy it,’ Sitkosky said.”
Sitkovsky stresses the versatility of this mechanism in immune-mediated therapies, citing several successful clinical trials and new drugs for numerous diseases. “This mechanism has the unique capability to not only be effective on its own, but boost the efficacy of other targeted therapies of cancer,” he said.
Image courtesy of Wikimedia Commons