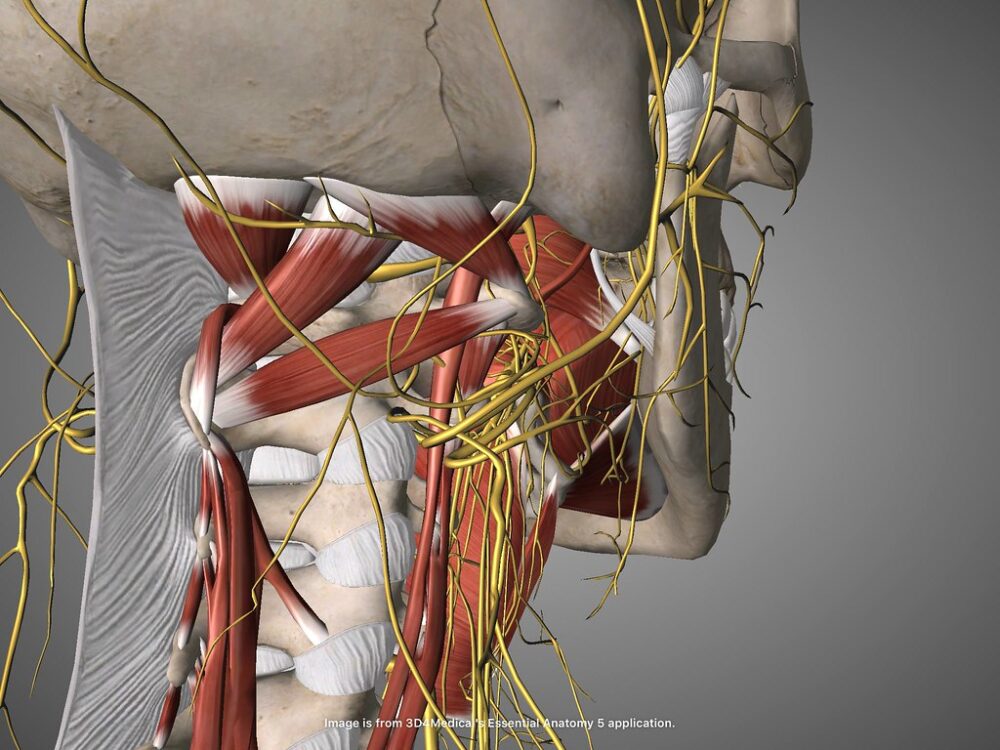
With hundreds of bones and muscles, thousands of genes, and trillions of cells, the human body is extremely intricate and specialized. The tenth cranial nerve, the vagus nerve, has recently come under the research spotlight due to its involvement in many different bodily functions. Nicknamed “the wanderer,” the vagus nerve is the longest and most complex cranial nerve. Unlike its counterparts, it has branches extending from the brainstem to the entire body, playing a key role in maintaining homeostasis.
Vagus nerve stimulation, or VNS, has been used since the early 2000s to treat various conditions like epilepsy, obesity, pain, and migraines, but its applications are still being explored. For example, a program called SPARC (Stimulating Peripheral Activity to Relieve Conditions) is searching for new therapies to treat other illnesses such as long COVID, rheumatoid arthritis, and inflammatory bowel disease. These solutions are all possible due to the vagus nerve having a hand in so many functions and processes.
One of which is regulating inflammation, the immune system’s natural response to damage or invasion by bacteria. However, if this response isn’t properly regulated, chronic inflammation can occur and lead to harmful effects on the body. A study by Aidan Falvey’s lab explored how stimulating the vagus nerve can regulate inflammation while also maintaining normal vital signs. Using mice in a sepsis model, they found that electrical stimulation of the vagus nerve’s dorsal motor nucleus (eDMNS) could decrease inflammation and increase the survival rate without negatively impacting heart rate. The results from Falvey’s lab are affirming, because it was the first regimen of eDMNS that could regulate inflammation without having adverse effects. Further research can investigate other conditions characterized by excessive inflammation.
“The medical applications of the vagus nerve can lead to more personalized solutions and better overall health for many.”
The vagus nerve’s role in inflammation regulation and the use of VNS to treat epilepsy has recently sparked an expansion of bioelectronic treatments for other conditions such as depression. A team led by Paul Lespérance tested the effects of VNS on six individuals with refractory depression, meaning they didn’t respond to multiple types of antidepressants. They did this by looking at the number of biomarkers in plasma molecules before and after VNS treatment. Biomarkers are measurable substances that can be used to predict the presence of a disease or other condition. They also examined proteins involved in the blood–brain barrier.
The severity of depression and anxiety were both significantly reduced following VNS treatment, and the numbers of several inflammation biomarkers and blood–brain barrier proteins were altered. These results shed light on the mechanisms of inflammation reduction and are a stepping stone for more research into using VNS to treat depression.
Moving further down the body, the vagus nerve is also critical in digestion and the gut microbiome. While it was already known that the vagus nerve helps maintain gastric homeostasis by monitoring hunger and feeling satisfied, a study by Sophie Müller and her lab used a particular type of VNS called transcutaneous auricular vagus nerve stimulation (taVNS) to increase the stomach-brain connection. It differs from standard VNS because it’s noninvasive; rather than being surgically implanted, taVNS is attached to the outside of the ear. taVNS has previously been found to improve motivation, memory, and mood. The researchers collected EGG and fMRI data before and after taVNS treatment. The results showed that taVNS can modulate stomach–brain communication and energy homeostasis.
The vagus nerve has a myriad of roles in the body, including mental health, immune response regulation, and digestion. Discoveries in one discipline inspire possibilities in others, and allow for the use of techniques like VNS to treat various conditions. By targeting specific groups of fibers on the vagus nerve, researchers hope to develop therapies and treatments for Parkinson’s disease, Crohn’s disease, traumatic brain injury, and even pain management. The medical applications of the vagus nerve can lead to more personalized solutions and better overall health for many.