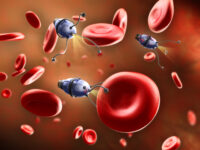
Among the many increasingly complex medical developments made since the start of the twentieth century, one discovery stands out among all the rest: antibiotics. Today, antibiotics may not seem to be such a wonder, yet their discovery — beginning with the isolation of penicillin in 1928 — has been revolutionary to medicine and global health. In the United States, antibiotics single-handedly changed the leading cause of death from communicable, infectious diseases to non-communicable diseases, including cardiovascular disease, stroke, and cancer. However, despite the overwhelmingly positive clinical outcomes, antibiotics may lose efficacy due to an emerging threat: antibiotic resistance (AMR). The antibiotics that have been successfully prescribed for decades are becoming increasingly less effective due to genetic mutation and the inheritance of resistant genes vertically and horizontally through species. Not only does this pose a serious public health threat, but due to the evolving nature of the problem, current solutions are scarce and mostly unsustainable.
At a microscopic level, numerous factors influence a strain’s ability to become resistant to antibiotics. While some strains of bacteria are naturally resistant to specific antibiotics, others gain resistance through genetic mutation or horizontal gene transfer. Genetic mutations include drug inactivation and alteration of the target binding site. Bacteria, like all organisms, evolve to promote the long-term survival of the species. By inactivating the bacterium’s intracellular enzyme that is targeted by antibiotics, the bacteria lose susceptibility.
In the United States, antibiotics single-handedly changed the leading cause of death from communicable, infectious diseases to non-communicable diseases, including cardiovascular disease, stroke, and cancer.
Similarly, bacteria can change the target binding site to which the antibiotic binds on the bacterium cell body. Mutations such as these are then passed onto offspring, making progenies equally as impervious. Moreover, bacteria can horizontally transfer genetic information, a process in which they convey genes to other bacteria that are not their offspring.
Despite genetic circumstances that have permitted bacteria to become such resilient organisms, humans have played a role in the accumulation of AMR as well. As Alexander Fleming, the man who discovered the first antibiotic (penicillin), correctly predicted “the public will demand [the drug]…then will begin an era…of abuse.” Numerous countries have no regulations on the use of antibiotics, leading to overuse. Contributing to the overuse of antibiotics is the incorrect application of them; it is estimated that 30 percent to 50 percent of cases in which antibiotics were used were either the wrong prescription or superfluous altogether, according to a 2015 article in Pharmacy and Therapeutics. With every low dosage of antibiotics prescribed, there is a risk of the strain receiving a genetic mutation that promotes resistance. Another major factor contributing to increased AMR is our use of antibiotics in the agricultural industry. Additionally, according to the 2015 article, approximately 80 percent of antibiotics sold are used in livestock to aid growth and prevent infection – livestock which is then consumed as food by humans. Thus, AMR transpiring in livestock is consequently transferred to humans.
While some strains of bacteria are naturally resistant to specific antibiotics, others gain resistance through genetic mutation or horizontal gene transfer.
Many countries, realizing the threat AMR poses, have started implementing various regulations on antibiotic use for livestock. The European Union has effectively seen a decline in rates of AMR due to these regulations, and, despite these trends, the United States has instituted far fewer parameters on antibiotic use than necessary.
Educating patients, the general community, and more thoroughly educating clinicians on the dangers of AMR is also a necessary measure to stop the inappropriate use of antibiotics. Education should also include information about preventative measures, such as the importance of vaccines, good personal and food hygiene, and environmental health. For clinics and hospitals, academic stewardship programs have been proposed, which are programs that would implement improved methods of care that would subsequently lower infection rates (and thus the need for antibiotics).
Approximately 80 percent of antibiotics sold are used in livestock to aid growth and prevent infection – livestock which is then consumed as food by humans. Thus, AMR transpiring in livestock is consequently transferred to humans.
Lastly, research and the development of new antibiotics have been a focal point of the AMR crisis. Until now, many research institutes and pharmaceutical companies have been responding to resistant strains of bacteria by developing new antibiotics that can target a species of bacteria. However, this solution is unsustainable due to high costs and the low financial reward correlated to this endeavor. The FDA must get involved to facilitate the research and development of antibiotics and improve the ambiguous guidelines that exist for clinical trials.
Despite the general resilience of bacteria, humans play a significant role in promoting resistance, and until we can successfully inhibit resistance among bacteria, we must change our policies, regulations, and methods of care in the interest of global health and human longevity.
Annals of Ibadan Postgraduate Medicine (2016). PMCID: PMC5354621
Clinical Infectious Diseases (2013). DOI: 10.1093/cid/cit070
Pharmacy and Therapeutics (2015). PMCID: PMC4378521