Since the emergence of modern Homo sapiens, humans have evolved and continue to evolve every day. Humans are getting smarter and more innovative, and are adapting better to our changing environment. But we’re not the only species that is evolving.
Candida auris, a type of fungi found in yeast, is known to cause candidiasis — a yeast infection typically on the skin, mouth, throat, gut, or vagina These yeast infections are typically not serious and are fairly common, as the yeast can live inside the body without causing problems. However, if this infection enters the bloodstream, known as invasive candidiasis or candidemia, it can be life-threatening. For patients who have long hospital stays and are constantly having medical devices being inserted into their skin, the infection is much more common. Treatment is usually antifungal medication, which for mild cases of candidemia can take around two weeks. For more severe instances, treatment may need to be continued for several weeks, especially if the infection has also tainted the heart, bones, or central nervous system.
C. auris infections have emerged globally, in countries like India, South Africa, Kuwait, Malaysia, England, and the United States. Researchers from bioMérieux Inc. found an upsurge in the detection of C. auris infections between 2021 and 2023, with the average detection rate rising from 0.014% to 0.057%.
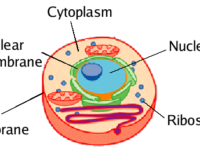
It was found that C. auris has evolved to become multidrug resistant. The biology behind C. auris’s resistance is fairly well understood, and a paper published in the Journal of Clinical Microbiology by Emily Spivak and Kimberley Hanson from the University of Utah explores these biological mechanisms behind the resistance. They cite the overexpression of multidrug transporters, mutations in an enzyme called lanosterol demethylase, increased expression of gene ERG11, and an alteration in the biosynthesis pathway that results in the replacement of ergosterols by other sterols in the cytoplasmic membrane.
Due to the resistance of C. auris, antifungal medications are not always successful, and in the future, treatment may be even less successful. Current efforts by researchers look toward preventing the contraction of the fungi in clinical and hospital settings. Specifically, as the spread of this fungi is often through surfaces and skin, good hand hygiene is critical, according to the Cleveland Clinic.
Additionally, research to find new treatments is ongoing. For example, Elizabete de Souza Candido and her lab at Dom Bosco Catholic University in Brazil investigated the use of echinocandins, which are a type of antifungal medication, as biotechnological tools for treating C. auris infections. The team of researchers found that echinocandins showed promise as a novel treatment, but more research still needs to be done.
“Overall, research to combat C. auris infections and candidemia will require the collaboration of public health, infection control, clinic and hospital settings, and biological labs.”
Overall, research to combat C. auris infections and candidemia will require the collaboration of public health, infection control, clinic and hospital settings, and biological labs. It will be difficult to work against the evolution of C. auris, and its resistance will likely mean that researchers will constantly need to create new antifungal medications to address the continually evolving variants.