Monkeys can play video games with their minds. Rats can control each others’ brains. Previously injured humans can restore sensation and function in limbs. These impossible-sounding events are all achievable with brain-computer interfaces (BCIs), which are systems that use electrical devices to collect neural signals from the central nervous system and, using algorithms, translate them into commands that operate output devices like computers or robotic limbs. There are ample cutting-edge applications of BCIs, but their biomedical applications have thus far been the most thoroughly studied.
“So far, BrainGate has allowed clinical trial participants to move cursors, robotic arms, and a previously paralyzed limb by simply thinking about movement.”
Because they are still in their experimental stages or currently being tested in clinical trials, their long-term effects have not been well-known, that is, until recently. A study published in Neurology early this year offers insight into the safety profile of such devices and optimism that they are feasible for widespread therapeutic use in the future.
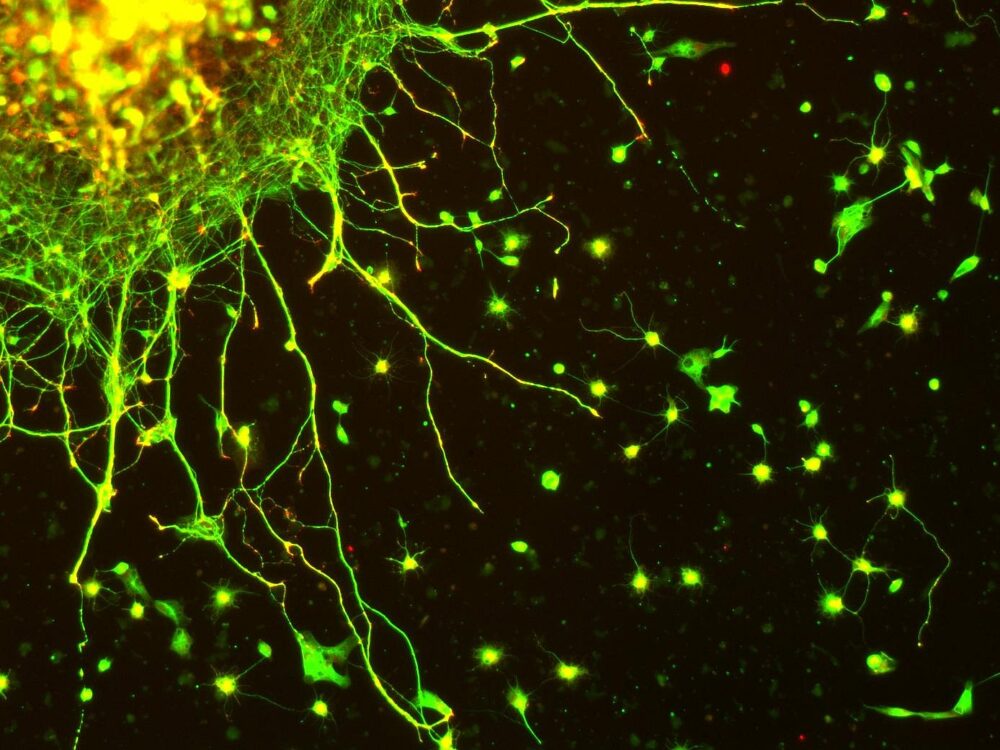
In the study, researchers from multiple institutions provide a comprehensive analysis of almost two decades of clinical trial testing for BrainGate, a leading neural interface system that uses a surgically implanted device to help those affected by paralysis, strokes, spinal cord injury, or other neuromuscular disorder regain control over their limbs. In the system, a microelectrode array smaller than a contact lens is attached to the surface of the motor cortex, the area of the brain that controls limb movement. The device gathers neural signals associated with body movement and subsequently sends them to a computer for decoding, which then controls an output device. So far, BrainGate has allowed clinical trial participants to move cursors, robotic arms, and a previously paralyzed limb by simply thinking about movement.
Researchers analyzed data regarding the safety outcomes of 14 participants aged 18–75 that participated in the ongoing clinical trial and reported a favorable risk-benefit ratio. The data showed that there were a total of 68 adverse events caused by patients’ use of the device from 2004–2021. The most common minor adverse event was skin irritation around the implantation site, but six of the events were serious. Two participants with a history of traumatic brain injury reported postoperative seizures, but they were easily treated. None of the six events resulted in increased disability, death, or device removal according to the researchers. Overall, data revealed low rates of adverse effects and showed that BrainGate’s safety is similar to that of other implanted neurologic devices such as deep brain stimulators or responsive neurostimulators. The researchers say this finding, along with recent performance advancements, supports continuing development of the technology.
“The golden day would be when somebody who is paralyzed gets a BrainGate-like system implanted, and they go play basketball.”
This report has drastically increased optimism that future widespread use of implantable BCIs as therapeutic devices will be possible. After its publication, Dr. Leigh R. Hochberg, a brain science professor and engineer at Brown University, stated that “Intracortical brain-computer interfaces have so much promise for restoring communication and mobility … The interim safety profile reported today supports the possibility that these systems may become restorative neurotechnologies for people with paralysis.”
Although there is much more work to be done, BrainGate researchers’ goal is for BCIs to eventually be fully implantable and available to all users at all times. John Donoghue, professor of neuroscience at Brown University and one of the principal BrainGate pioneers, explains that “The golden day would be when somebody who is paralyzed gets a BrainGate-like system implanted, and they go play basketball.” After the recent publication of the safety report, it is promising that this golden day may soon become a reality.