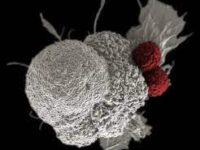
Every second of the day, the body fights a battle using a remarkable defense mechanism, neutralizing harmful invaders to ensure health and well-being. The human immune system is a powerful defense mechanism used to protect the host from pathogens or foreign invaders. During pregnancy, the woman’s decidua, the layer of tissue in the uterus supporting the embryo and placenta during pregnancy, has a great number of immune cells to accommodate the developing fetus. These cells at the fetus implantation site work to protect the baby, rather than treating it as a foreign body.
The maternal immune defense and capacity to persist cooperate in a carefully regulated environment. Throughout pregnancy, a mother’s body can become more susceptible to various illnesses as a result of the immune system’s preoccupied efforts to prevent the fetus from being identified as a foreign body. At the same time, the fetus makes a contribution by establishing its own immature immune system, resulting in a unique interaction that allows pregnant women to display different immune responses to pathogens.
The placenta, which acts as a physical and immunological barrier, is one of the primary factors in this immune response. The placenta plays a role in immune defense by generating antimicrobial peptides and expressing toll-like receptors (TLRs) such as TLR-3, TLR-7, TLR-8, and TLR-9, which detect pathogens to activate the body’s immune response. For example, in the first trimester, two antiviral agents stimulate trophoblast cells. The stimulation of this intracellular defense mechanism aids in protecting the embryo from viral infections. This highlights the placenta as an active immune organ that recognizes and responds to pathogens. Its susceptibility to infections shows its uniqueness during pregnancy, as these infections would not occur in a non-pregnant state.
“This highlights the placenta as an active immune organ that recognizes and responds to pathogens.”
Researcher Tippi MacKenzie from UC San Francisco further highlights the necessity required to protect the mother and fetus during pregnancy. Results show that under normal conditions, the fetal immune system remains inactive, allowing the pregnancy to progress without immune conflict. This interaction between the mother and fetus during pregnancy corresponds to the tolerance required for organ translation, where the immune system must regulate itself to avoid rejection. Specialized immune cells called regulatory T cells (Tregs) control this and are essential in suppressing potentially dangerous immunological reactions. By influencing other T cells that may otherwise target fetal cells, Tregs prevent the mother’s immune system from treating the fetus as a foreign body throughout the pregnancy. This ensures that the fetus can grow in a safe environment.
The study’s conclusion provides light on what occurs when this critical balance is disrupted. Normally, the fetal immune system depends on the mother’s Tregs to keep it from being rejected because it is still immature. Inflammation brought on by the mother’s sickness can disturb this balance and cause the fetal immune system to be activated prematurely. This can lead to increasing immune responses, potentially interfering with normal fetal development and leading to an inflammatory reaction that causes preterm labor and uterine contractions. In the end, maintaining an intricate balance between the mother and fetal immune systems is crucial for a healthy pregnancy, while protecting the mother and allowing for safe development of the baby.