Revolutionizing HIV
By Ololade “Lola” Akingbade, Behavioral Neuroscience, 2018
One of the largest public health crises facing our nation is HIV/AIDS. HIV, human immunodeficiency virus, is characterized by a progressive failure of the immune system, and can lead to acquired immunodeficiency syndrome, or AIDS. There is no current effective cure. As a global pandemic, 35.3 million people live with HIV globally, with 68 percent of these cases in Sub-Saharan Africa. Domestically, the United States served as the center of the 1980s AIDS epidemic, first observed in young metropolitan LGBTQ populations. Currently 1.2 million people in the United States live with HIV, and 1 in 8 are unaware of their infection. Rates of diagnosis are higher in Black Americans, consisting of 43 percent of all cases in the U.S.
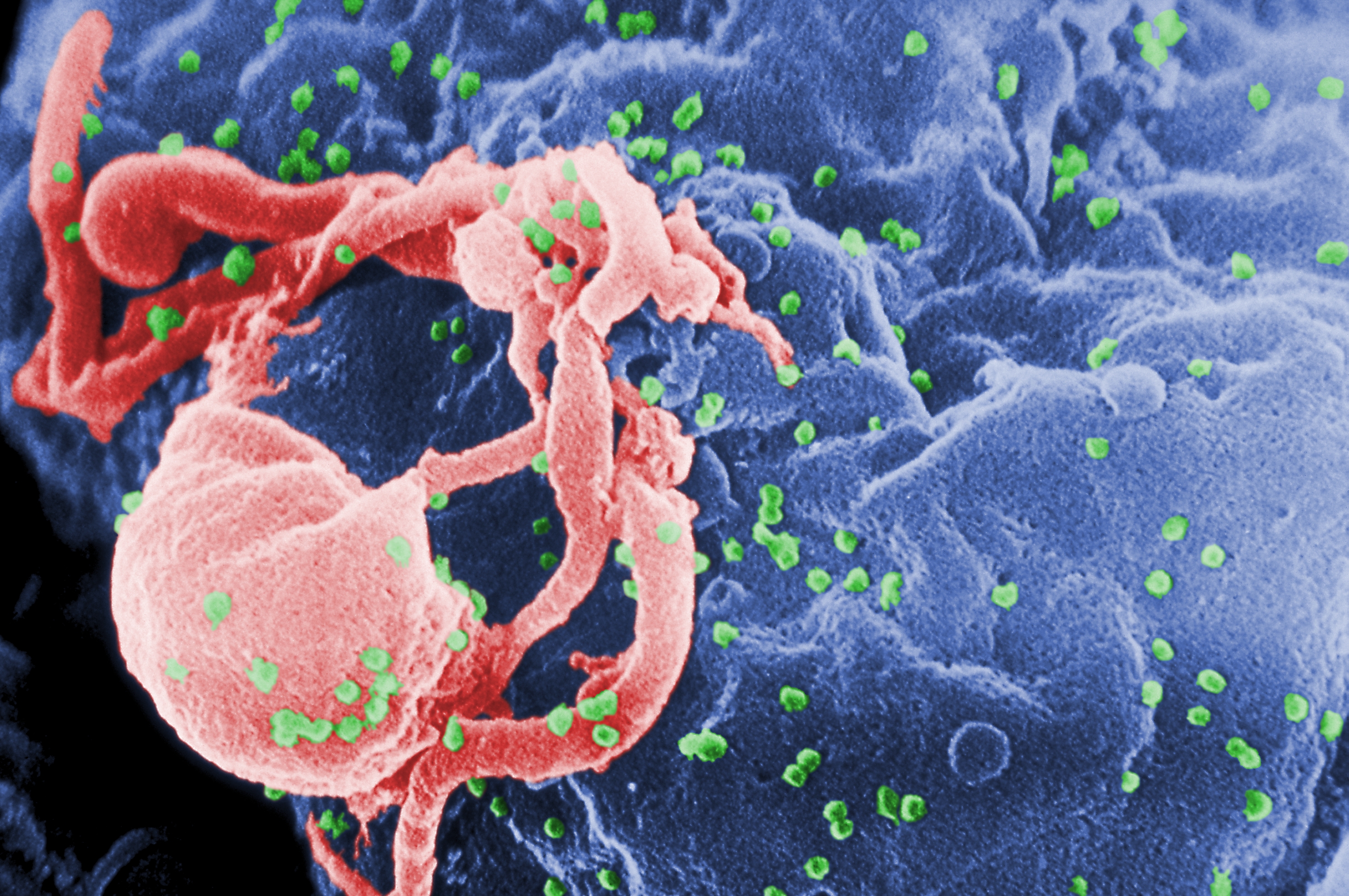
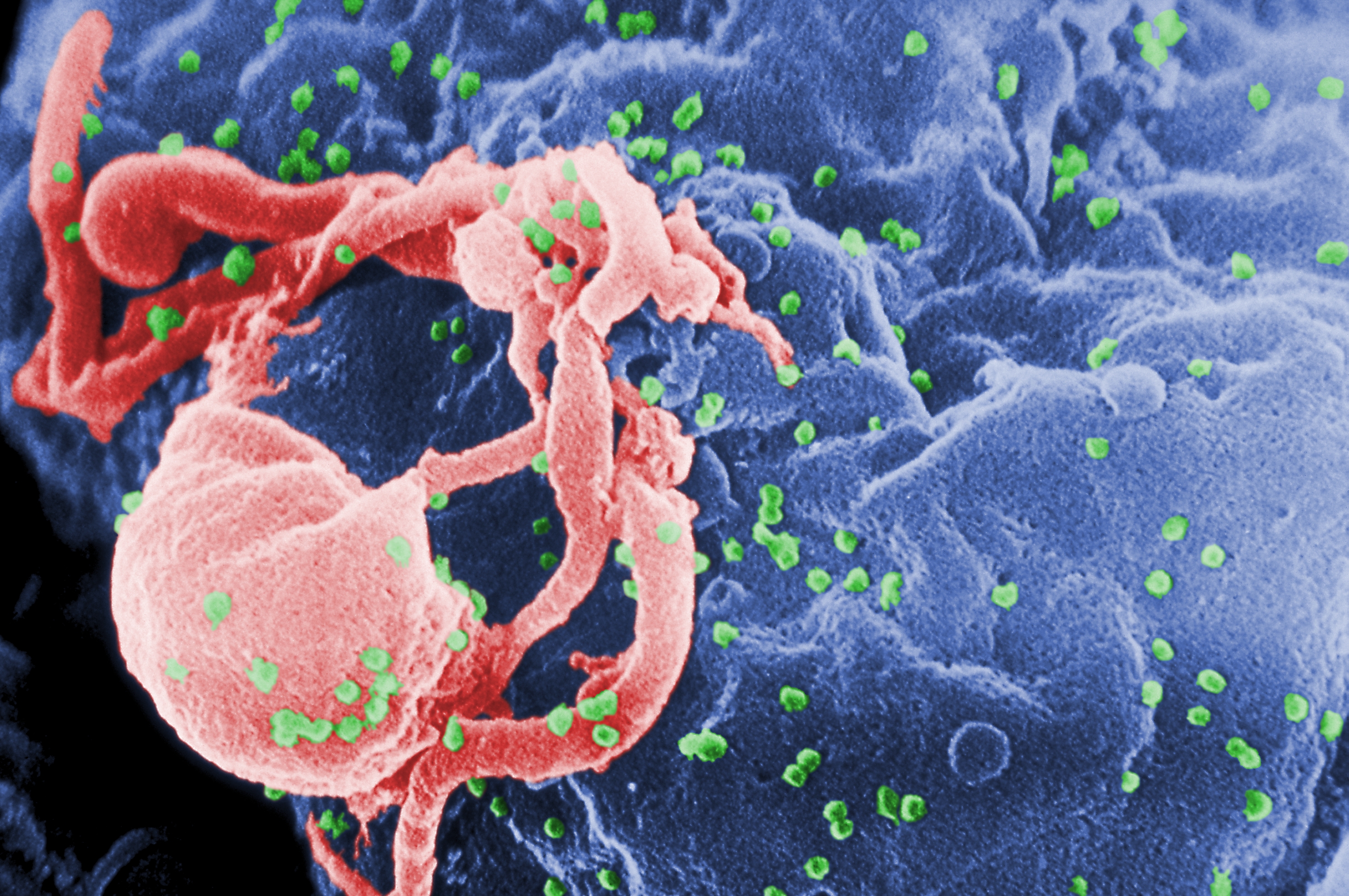
HIV’s profound social implications and prevalence are underscored by complex biological characteristics. The disease spreads by lentivirus transmission, when a single stranded RNA virus is reverse transcribed into double stranded DNA and integrated into a cell’s nucleus. HIV transmits between parties through bodily fluids and affects white blood cells in the immune system, specifically CD4+ T cells.
Pathologically, HIV begins with an acute infection characterized by flu-like symptoms. As the disease transitions into clinical latency, HIV reproduces at low levels, often presenting itself asymptomatically. Proper treatment in this stage is definitive in determining disease progression: with proper HIV treatment, latency can continue for decades to limited ill effect, while without treatment, the disease progresses. AIDS develops once CD4 immune cell count is low — fewer than 200 cells/mm3 — and opportunistic infections thrive.
Although HIV is more easily diagnosable and treatable than it was in decades past, its chronic nature calls for costly disease management. Today’s drugs work by reducing viral load, the amount of HIV in the blood. Antiretroviral Therapy (ART), prevent growth of the HIV disease, usually through reverse transcriptase inhibition or inhibition of various steps in the HIV life cycle. Viral load daily treatments are hard to keep routinely and get access to, especially for low income. Long-acting HIV management shots are more easily administered than daily pills, allowing for consistency in treatment regime. Such regime could change healthcare for patients with HIV.
A study conducted by ViiV Healthcare in collaboration with Johnson and Johnson, GSK, and Pfizer, entitled the Long-Acting Antiretroviral Treatment Enabling study, shows promise in the area of long-acting HIV treatment. A shot once every 1 to 2 months was found to be as effective as daily pill treatment for HIV. Now injection of two drugs that suppress HIV and AIDS every 4 and 8 weeks works just as well as 3- a-day pill treatment. As a Phase 2b study, these findings are pivotal to treatment efficacy and are crucial in defining dose range for patients.
The trial’s monthly treatments centered on the drugs Cabotegravir and Rilpivirine, created by Viiv and Johnson and Johnson respectively. Rilpivirine blocks the reverse transcription process and can be administered via injection. Cabotegravir works against infection, blocking integrase, an HIV enzyme that integrates viral DNA into human cell DNA. As these treatment options progress into phase 3 testing on larger patient groups, John Pottage, the chief medical officer for ViiV, expects U.S Food and Drug Administration approval soon after. As of now, ViiV has found the long-term treatment to be as effective as daily pills, achieving a 94 percent and 95 percent viral suppression rate successfully.
“When you think about people with HIV, you’re going to treat them for a lifetime, and you have to treat them with a combination of drugs,” Pottage said in an interview with Newsweek. “Monotherapy is not enough. There are patients who get tired of taking daily pills, or have lifestyles that don’t lend themselves to that.”
Apart from the time and convenience benefit of long-term drug treatment, this new regime could also lessen the financial challenges of HIV maintenance. Lifetime cost of care can total hundreds of thousands, averaging $14,000–20,000 per year. Close to 30 percent of those living with HIV and AIDS in the US have the disease under control through a medical treatment plan. More than 50 percent of those living with HIV/AIDS have costs covered by Medicaid and Medicare, but often times is not covered unless an individual has AIDS or is disabled by HIV.
“Going from many pills a day — like 10, 20 pills a day — to now one pill, to now one injection every two months is I think a huge medical technical achievement,” said Johnson & Johnson Pharmaceutical Chairman Paul Stoffels in an interview with Bloomberg News. “Long-acting injectable drug formulations may offer another option for HIV maintenance therapy.” The developers are looking to bring long-lasting injection treatment to the market by 2019, which could positively change health outcomes and the economic issues behind effective HIV treatment.
