Modern scientists rely heavily on cell culture in laboratories to understand how cells work in order to provide possible cures for diseases. Brain cells are some of the most difficult cells to study simply because there’s a lack of access. Scientists have been able to grow brain cells previously by use of induced pluripotent stem cells (iPSCs). iPSCs are cells created in a laboratory that take skin or blood cells and use human transcription factors to turn the cell into an embryonic-like stem cell. An embryonic-like stem cell can differentiate into any type of cell in the human body, including neurons. This is one way that scientists have been able to grow neurons in culture without needing human tissue samples.
The only problem is that cells in a culture do not always act in the same way as cells in a human body. Cells in the human body receive different nutrients via the bloodstream and cell-to-cell interactions that cells in culture cannot receive. Cells in culture tend to have trouble maturing in the same way. These cells also cannot integrate into a system to generate behavioral outputs. This creates a limitation when looking at neuropsychiatric diseases because scientists cannot yet understand those processes in a laboratory. As of this year, however, scientists may have found a solution to overcome these limitations.
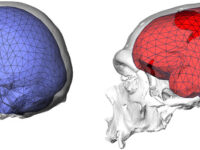
Recently, scientists have successfully implanted human neurons in newborn rat brains. According to Omer Revah, a scientist in the Department of Psychiatry and Behavioral Sciences at Stanford University, and his colleagues, not only has the implantation of these neurons been successful, there is evidence that these new cell types “integrate into sensory and motivation-related circuits.” These cells display much more complex properties than neurons grown in culture.
In order to test whether this rat model could be an option for studying disease phenotypes, the scientists implanted cells from patients with Timothy Syndrome (TS). TS is a rare, life-threatening genetic condition that affects the brain as well as the heart, the immune system, and the phalanges of a child. The mutation, found in the Cacna1c gene that builds a protein associated with calcium ion transport, can affect a child’s brain development tremendously. In this study, not only did these cells mature in the rat brain, the rats implanted with TS cells showed defects in neurons just as they would in a human. This finding could possibly open the door for in-depth studies of brain development and brain disorders through rat brain modeling. If scientists can continue to implant cells of different brain disorders into rat brains and continue to see the correct phenotype, this can lead to a whole new aspect of study in the fields of both neurology and psychiatry.
In addition, these scientists studied whether the rats with human neurons could drive reward-seeking behavior. In order to do this, they first implanted human neuron cells that expressed a light-sensitive cation channel, channelrhodopsin-2, which made the rats more reactive to blue light. Then they trained the rats by rewarding them with water if they licked during a blue light rather than during a red light. After a little over two weeks of this practice, the rats were beginning to show increased licking during the blue light rather than the red light. This behavior change was not observed in rat brains that were implanted with neurons that did not express the channelrhodopsin-2. This demonstrated that the human cells implanted in rat brains can communicate with rat neurons in order to drive reward-seeking behavior.
“Human cells implanted in rat brains can communicate with rat neurons in order to drive reward-seeking behavior.”
Overall, this study shows that neurons can mature in rat brains and integrate themselves into the phenotype. By demonstrating the rat’s ability to seek rewards for certain behaviors, it shows the ability of the human neurons to connect and influence rat neuron activity. In addition, the prospect of being able to produce disease phenotypes such as TS in rat models could provide amazing new disease research in the coming years. This study is the beginning of a very promising new laboratory technique and could possibly open up studies for diseases that before were quite limited.