Researchers at MIT have developed a novel approach that has the potential to increase the accuracy and efficiency of early lung cancer detection. The new diagnostic test is based on nanosensors, capable of entering the body via an inhaler or nebulizer, and a strip-based paper urine test that can identify DNA barcodes associated with particular lung cancer-linked proteins.
The technology could potentially replace or supplement the leading biomedical process used for lung cancer diagnosis: low-dose CT scans. Known to decrease mortality in those with a high risk for cancer, these non-invasive scans function as special X-rays that take multiple pictures of the subject’s chest as they lie on a table and slide in and out of the CT machine. Despite CT scans’ popularity and delivery of accurate results over the years, nanosensors, combined with the paper urine test, can serve as an accurate and reasonably priced alternative for underprivileged populations in low- and middle-income countries.
“The epidemiology of lung cancer globally is that it’s driven by pollution and smoking, so we know that those are settings where accessibility to this kind of technology could have a big impact,” Sangeetha Bhatia told MIT News. Bhatia is a professor of Health Sciences and of Electrical Engineering and Computer Science at MIT, and a member of MIT’s Koch Institute for Integrative Cancer Research and the Institute for Medical Engineering and Science.
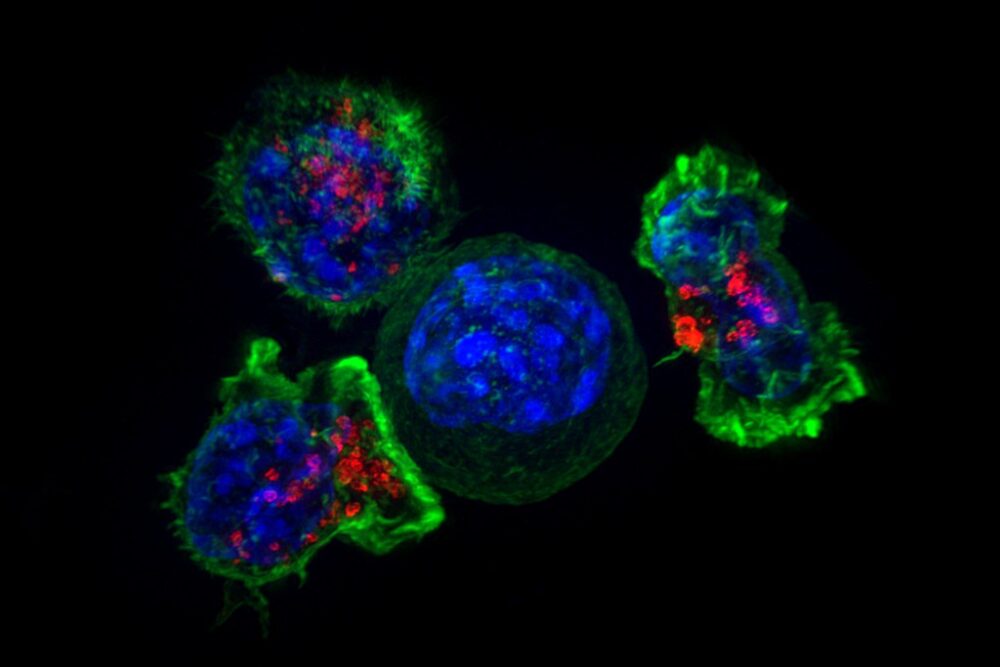
Bhatia’s lab has spent the last few years developing nanosensors to improve early lung cancer detection. Their study involved coating polymer nanoparticles with a reporter such as a DNA barcode, which can be cleaved from the particle when the nanosensor locates the protease enzyme in cancer-associated proteins. Considering that these enzymes are identified by their overactivity in tumors, the DNA reporters are responsible for tagging cancer-linked proteins and eventually accumulating in the individual’s urine.
While previous versions of the sensors were designed to be inserted through the veins and utilize mass spectrometry to analyze urine samples, the team was keen on creating a version of the sensor that could be inhaled in order to increase accessibility in resource-deprived areas. With that consideration in mind, a lateral flow assay was developed to detect four specific DNA barcodes, using a paper strip.
“We were really pushing this assay to be point-of-care available in a low-resource setting, so the idea was to not do any sample processing, not do any amplification, just to be able to put the sample right on the paper and read it out in 20 minutes,” Bhatia told MIT News.
The system was tested in mice that were genetically engineered to develop tumors similar to those observed in humans. In the first set of experiments, the scientists administered the sensors to the mice after 7.5 weeks since this time period aligns with stage 1 or 2 of cancer in humans. Although 20 distinct sensors were used to detect different proteases, the team was able to identify four particular sensors that accurately detected the early-stage lung tumors in the experimental mice. While it is possible that humans may require a greater number of sensors for an accurate diagnosis, using four or more paper strips — each of which detects four or more different sensors — can achieve the same results as the study.
As a next step, the researchers plan on analyzing human biopsy samples to verify that the sensors work as expected when detecting human cancers. In fact, a company called SunBird Bio has already run phase 1 trials on a similar sensor developed by Bhatia’s lab, which proved to be useful in diagnosing liver cancer and nonalcoholic steatohepatitis (NASH).
“The CT scan is a good tool that can see a lot of things,” she told MIT News. “The problem with it is that 95% of what it finds is not cancer, and right now you have to biopsy too many patients who test positive.”
“In a fast-paced, technologically advancing world, Polaris Market Research predicts that the global market for disposable medical sensors is expected to grow from $10.4 billion to $42.4 billion in 2032, representing a 16.9% annual growth rate over the next decade.”
In a fast-paced, technologically advancing world, Polaris Market Research predicts that the global market for disposable medical sensors is expected to grow from $10.4 billion to $42.4 billion in 2032, representing a 16.9% annual growth rate over the next decade. With adequate funding, inhalable nanosensors have the potential to reduce the resource threshold for cancer detection; enhance cancer screening and detection tools to provide a more rapid diagnosis and treatment; and improve global health by providing underprivileged populations with a reasonably priced, simple-to-use, and efficient alternative.