“Hemorrhage is the number one potentially preventable death.” Curtis Conklin, Command Surgeon for the U.S. Armed Forces Command (FORSCOM), echoes in a statement to NU Sci what has already been emphasized for decades: the issue of blood supply, from the floors of hospitals to the fields of duty. Luckily, a recent advance in hematology called ErythroMer has the potential to ease unmet demands for blood.
“Hemorrhage is the number one potentially preventable death.”
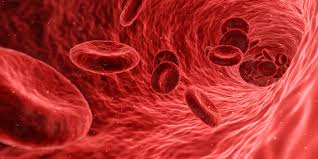
Hemorrhage is defined as “acute blood loss from a damaged blood vessel.” If blood loss is great, vital tissues in the body enter hemorrhagic shock from lack of oxygen, resulting in death. Command Surgeon Conklin cites hemorrhage as the leading cause of preventable death in the field, extremity hemorrhage in particular. Wounds inflicted in combat typically result in some degree of hemorrhage, and, if left untreated, even a small bleed may compound and result in death.
It is for this reason that the top priority in the event of injury is to control or stop bleeding. The standard method is with the Combat Action Tourniquet (CAT), a simple device that functions like a ratchet to tighten adjustable straps around the source of bleeding. Because access to advanced treatment in a battle zone is often not immediate, all soldiers carry a small first aid kit on their person containing such a device. They are trained to use it on whomever may require it–whether it be a fellow comrade or themselves.
The next step in treating hemorrhage after stabilizing a wound is replacing fluids and/or replenishing blood volume. Sometimes this is available in the field, sometimes not—a patient might have to wait until a Pararescue team–an emergency team for the military–can reach them, or until they can be transported to an established medical facility.
Whole blood is generally in short supply on the field. Even when available, it remains a volatile resource: blood may be carried in small coolers for travel, but these coolers must be carefully regulated. If various environmental factors (including temperature) fluctuate outside of designated standards, the blood is no longer considered viable for use.
This fact also reduces the potential amount of blood that can be transported at a time. Pararescue teams, who frequently operate in groups of twelve, can carry 2 pints with them. A smaller team of six carries only one. Thus, field medics must make critical decisions in allocating blood to patients with the best chance of survival.
Even blood available at established medical facilities is limited. The U.S. Military strictly follows a 31-day shelf-life, and the process of shipping blood across the world eats into valuable time it can remain at a facility before it must be discarded. “Supply and demand is a delicate dance,” acknowledges Command Surgeon Conklin, noting that every attempt is made not to waste blood. Such efforts include strategies like allocating the oldest blood to units with the highest use rate. Blood waste does not necessarily mean that demands are being met, though—especially when there is already a supply crisis on the home front.
“Walking blood banks,” a list of predetermined donors for on-demand donation, are the current source of reserve supply when whole blood is unavailable. These donors have undergone prior testing to ensure they meet the standard for donation, and if necessary are called upon in the field for blood to be drawn and immediately readministered to a patient. Though the process is now relatively streamlined (under 12 minutes), on-demand transfusions previously took up to 45 minutes in the absence of a pre-established list of donors. A potential donor would need to be blood typed in the field and pass a titer test, which requires several minutes and sterile conditions. Only then could a transfusion begin.
The process was slow and cumbersome, making it unsuitable for the field of combat and an unreliable fallback for whole blood. Even still, it is still not a sufficient supplement to meet the demand for whole blood. However, a new Defense Advanced Research Projects Agency (DARPA) initiative aims to meet demands in a new way. Last year, DARPA committed $46 million to the creation of the Fieldable Solutions for Hemorrhage with bio-Artificial Resuscitation Products (FSHARP) program, which aims to develop a field-deployable, shelf-stable whole blood equivalent.
Integral to this program is ErythroMer, a potential synthetic human blood substitute created by Dr. Allan Doctor at the University of Maryland School of Medicine. ErythroMer is one of the more successful of other hemoglobin-based oxygen carriers (HBOC). It is a synthetic, freeze-dried substance mimicking blood cells carrying hemoglobin that can be mixed with saline and introduced to a patient to replenish blood supply. Hemoglobin is a vital protein present in red blood cells, responsible for picking up oxygen in the lungs and carrying it through the bloodstream to deposit in tissues.
There have been prior attempts at a blood substitute, the earliest being perfluorocarbons and, more notably, Hemopure. The viability of these candidates was largely reduced by related side effects or manufacturing issues, and until ErythroMer, Hemopure remained the closest to a successful synthetic substitute.
What was special about Hemopure was that it was not really “synthetic” at all. It used hemoglobin purified from cow’s blood and reconstructed into hemoglobin tetramers, rather than synthesizing the protein from scratch. The major factor barring it from success was concerns about potential side effects, because the hemoglobin diverged from mammalian physiology in one key way: it was free-floating in suspension, not encapsulated within a cell membrane. The membrane of red blood cells is key in preventing oxygen bound to hemoglobin from reacting with (oxidizing) and damaging the wrong places in the body.
ErythroMer reflects the strengths of Hemopure and builds upon them. For one, the hemoglobin molecules in ErythroMer are not just mammalian, they are in fact recycled human hemoglobin molecules. Even better, they are recycled from previously-donated human blood that has exceeded its shelf life. Not only will this reduce blood waste, but it also ensures that viable whole blood is not taken from potential patients in order to produce the substitute.
The second, and perhaps more significant improvement, is the addition of a synthetic lipid membrane to enclose the hemoglobin molecules. This addresses the issue of oxidation posed by oxygen when it is not encapsulated by a membrane in the bloodstream. The presence of a synthetic membrane is even more important because it ensures that the substitute blood is not type-specific. Whereas human blood cells have specific surface proteins, allowing the immune system to distinguish between “self” and “other,” and subsequently react to anything not denoted as “self,” the ErythroMer membrane can be synthesized without any surface proteins at all, skirting the problem altogether.
Because it is reliant upon donated human hemoglobin, ErythroMer is still susceptible to similar supply and demand issues plaguing human blood. However, because it makes use of blood past its shelf life, this new substitute can still increase the overall availability of usable blood (or perhaps, blood-analogues) and reduce blood waste. It is currently only tested in animals, but perhaps the future of ErythroMer lies in combat zones, easing the many logistical issues currently faced by the distribution and use of whole blood. But regardless of its eventual fate, in the words of Former Air Force Pararescueman Frank Grun, “it is certain that a non-perishable, expendable artificial agent would save thousands.”