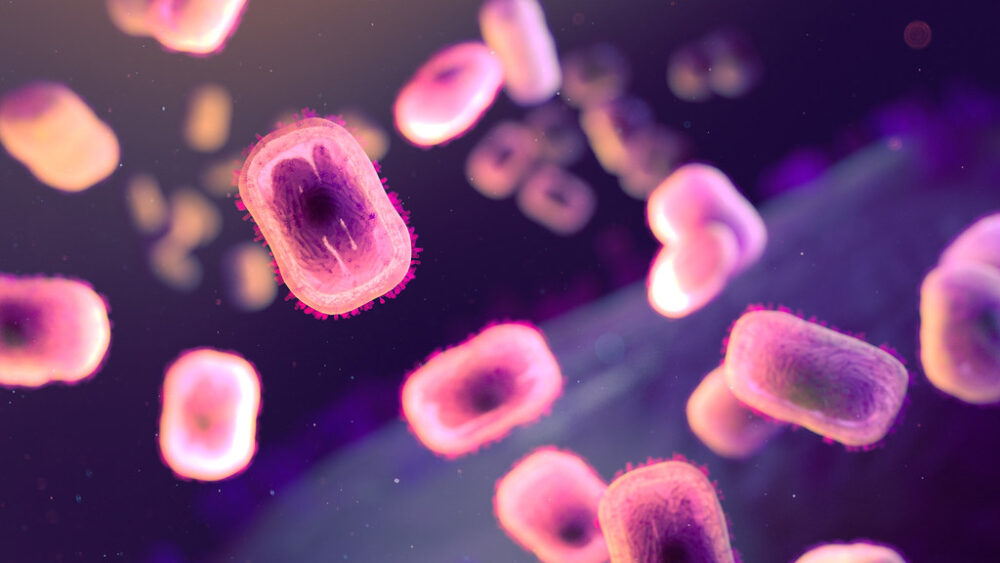
Just when the world thought it had gotten a grasp on COVID-19, monkeypox emerged as another infectious disease and public health concern. Monkeypox is a viral disease classified as an Orthopoxvirus, a genus that includes smallpox, cowpox, camelpox, and similar diseases. Excluding smallpox, all human cases of orthopoxviruses are considered zoonoses, or diseases transmitted to humans by animals. Monkeypox was first discovered in a monkey in a Danish lab in 1958, but contrary to what the name suggests, the virus is more common among rodents.
The disease is characterized by the rash it causes, which eventually develops into blisters and lesions — patients can have anywhere from a few lesions to thousands. Other symptoms include fever, headache, fatigue, and enlarged lymph nodes; people typically show symptoms for two to four weeks. Transmission often occurs via contact with an infected person’s lesions, bodily fluids, or respiratory secretions, but monkeypox can also be contracted by touching objects used by an infected person.
More severe complications are possible, including pulmonary distress, blindness, and even death. People at risk are immunocompromised individuals, pregnant women, and children under age eight. The mortality rate is around 10%, but this is likely a high estimate and result of the disease being more prevalent in regions with limited access to healthcare. Luckily, this is still significantly lower than smallpox’s mortality rate of 30%.
A crucial tool for controlling monkeypox is vaccination. Since the viruses are so closely related, the smallpox vaccine (widely administered in the mid-20th century during the smallpox eradication campaign) offers strong monkeypox protection. However, since smallpox eradication was achieved in 1980, this vaccination is no longer routine, leaving people vulnerable to monkeypox
The first human case of monkeypox was identified in 1970 in the Democratic Republic of Congo, and it has been an endemic (locally contained) disease in Central and West Africa for over 50 years. Virologists have noted migration into animal habitats as a cause, along with the high prevalence of HIV and AIDS in the region, which left much of the sub-Saharan African population immunocompromised and vulnerable. This, combined with the fact that smallpox vaccinations and immunity were waning, allowed monkeypox to thrive in Africa.
The current 2022 outbreak began in mid-May, marking the first time monkeypox spread widely beyond Africa. According to CDC data from October 2022, there have been nearly 70,000 confirmed cases in 107 countries, 100 of which have not historically reported monkeypox. The countries with the most cases this year are the United States with over 26,000, then Brazil with over 7,800, and France with around 7,100. Recently, the disease has been largely transmitted through sexual activity; the CDC reports that 99% of US monkeypox cases occurred in men, 94% of whom “reported recent male-to-male sexual or close intimate contact.” Disease statistics can be influenced by many biases, so it is critical that community health officials work in an equitable manner to minimize stigma and reduce barriers against prevention, testing, and treatment. Fortunately, very few cases of monkeypox have resulted in death throughout this 2022 outbreak, and treatments are generally effective.
Experts attribute the current monkeypox outbreak to improper disease monitoring and inadequate public health measures.
Experts attribute the current monkeypox outbreak to improper disease monitoring and inadequate public health measures. Monkeypox surveillance in Africa has not been consistent or adequate, enabling international spread. Additionally, monkeypox researchers have historically struggled to receive funding. Many important questions surrounding the disease still need answers, including the specifics of transmission, the severity for different risk groups, patterns of pre-symptomatic transmission, and the stability of the virus on surfaces and in air.
An especially important concern is reverse zoonosis, or the spreading of monkeypox from humans back to animals in new regions. The establishment of the disease in an animal reservoir (likely a rodent) in Europe or North America would make eradication nearly impossible.
Thankfully, antiviral drugs are useful and a monkeypox vaccine exists. One positive side effect of this outbreak is the fact that it allows scientists to assess their arsenal of treatment against orthopoxviruses. Monkeypox has historically been studied by researchers as a surrogate for smallpox, and the link between the two is yet another reason to support monkeypox research.
Diseases have complex odysseys, often with significant effects on global populations. It is crucial that scientists work to uncover as much information as possible and that healthcare becomes increasingly available and equitable. This way, both prevention and treatment are prioritized, drastically improving human health outcomes and limiting the scale of future outbreaks. Hopefully, these challenging past few years encourage scientists and policymakers alike to realize the importance of monitoring and controlling disease before it gets out of hand, and maybe someday, monkeypox can join smallpox as another eradicated disease.