Therapeutic hypothermia, as the name suggests, is a method of purposefully lowering a patient’s body temperature to approximately 93 degrees Fahrenheit in an effort to increase survival rate and decrease the likelihood of further damage to the brain.
Take for example, a patient who’s suffered cardiac arrest and, after an intense round of CPR, has been brought back from the brink of death. They now face brain death from a lack of oxygen for prolonged periods — or even the inflammation and swelling of the brain that comes with resuscitation as the body overcompensates and rushes to send blood through the veins and to all its tissues. For those who are recovering from a cardiac arrest, the risk of neurological damage is all too real — but recent research has brought therapeutic hypothermia to the forefront of medicine as a potential way to minimize that risk.
For those who are recovering from a cardiac arrest, the risk of neurological damage is all too real — but recent research has brought therapeutic hypothermia to the forefront of medicine as a potential way to minimize that risk.
The process of decreasing a patient’s internal body temperature is complex and calls for extreme precision. In the case of a patient who’s been revived after cardiac arrest, in the event that their temperature decreases below the desired point of 93 degrees, the patient may undergo arrest again. While the patient receives a cold saline solution infused intravenously and is cooled using a blanket which helps the saline solution spread throughout the veins to the rest of the body, one must keep a close eye on their temperature. Then, to minimize shivering that occurs after anyone’s temperature decreases enough, the patient must be sedated heavily and given measured doses of paralytic agents. If the patient were to shiver throughout the process, they would use up oxygen far too quickly; a flood of oxygen to the body and brain tissues, which have been without it for quite some time, would actually be detrimental to the patient as the excess could damage the aforementioned tissues. Afterward, the patient is kept in the intensive care unit for 24 hours — and only after is their temperature slowly increased and brought back to normal, their oxygen levels following in time.
Therapeutic hypothermia is quickly becoming a standard for post-resuscitative patient care throughout the world — and for good reason. According to a journal article published in the Scandanavian Journal of Trauma, Resuscitation and Emergency Medicine titled, “Therapeutic hypothermia for acute brain injuries,” the aforementioned therapy has an incredible usefulness in more than just cardiac arrest cases. Patients suffering from various types of strokes, hemorrhages in the brain, or physical trauma to the brain, among others, can also benefit from this treatment plan.
Patients suffering from various types of strokes, hemorrhages in the brain, or physical trauma to the brain, among others, can also benefit from this treatment plan.
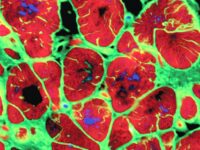
Though it has its drawbacks, such as a decrease in the rate of the body’s metabolism, which would usually kick in to supply oxygen from head to toe after asphyxia (a prolonged period without oxygen), most research agrees that the benefits are far greater. For example, when targeted temperature management is used, swelling of the tissues in the brain — which, if left uncontrolled, are a potential killer — can be greatly minimized. It can also decrease the likelihood of neurons being damaged or even killed permanently as a result of overstimulation of their receptors when reperfusion occurs in the body’s tissues. Therapeutic hypothermia can also keep ATP stores from depleting, prevent cell death, and even reduce the production of free radicals — unstable molecules, which, when produced in excess, can cause lasting damage to the body’s tissues.
However, despite all of its benefits, therapeutic hypothermia is most effective when begun immediately after a cardiac arrest or other brain injury. It seems to most experts that strengthening the chain of survival — that is to say, CPR, transport by emergency medical technicians (EMTs), and other post-resuscitative care that occurs in a hospital — as well as decreasing the time it takes for those steps to occur can be the difference between irreversible brain damage and a chance at a full recovery.
Scandanavian Journal of Trauma, Resuscitation and Emergency Medicine (2015). DOI: 10.1186/s13049-015-0121-3