In the world of medicine, the need for viable, healthy tissue and organs is critical. Yet, in the United States alone, over 100,000 patients are waiting for organ transplants, while many also struggle with chronic conditions requiring tissue regeneration. A promising solution lies in 3D bioprinting, a groundbreaking technology at the intersection of biology, engineering, and medicine that is reshaping the future of healthcare.
3D bioprinting uses digital designs to precisely deposit living cells and biomaterials, constructing functional tissues layer by layer. Unlike conventional 3D printers that use plastics or metals, bioprinters use bioinks composed of living cells, hydrogels, and growth factors. This allows researchers to print human–like tissues that could potentially replace damaged or diseased parts of the body. Kevin Dicker, a researcher at Mayo Clinic, and his team believe these bioprinters are tools to accelerate research in tissue engineering by pushing the boundaries of regenerative medicine.
“Bioprinted tissue models serve as advanced platforms for drug testing and therapy development, potentially reducing reliance on animal testing and expediting the discovery of effective treatments for conditions such as cancer and autoimmune diseases.”
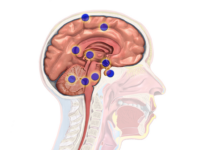
Among the most promising applications of 3D bioprinting is the creation of human organs. While fully functional printed organs remain in development, significant progress has been made at the Mayo Clinic where researchers have successfully developed bioprinted skin models that replicate human skin structure, facilitating research on conditions like eczema. These models allow scientists to test new treatments and understand how diseases like atopic dermatitis progress on a cellular level. Another team of researchers at Penn State University is experimenting with bioprinting bones, cartilage, and even muscle tissue, envisioning a future where doctors can print tissues directly onto patients to repair wounds or fractures without grafts. This approach could reduce complications and eliminate the risks associated with donor tissue rejection. The applications of 3D bioprinting extend beyond organ regeneration. Bioprinted tissue models serve as advanced platforms for drug testing and therapy development, potentially reducing reliance on animal testing and expediting the discovery of effective treatments for conditions such as cancer and autoimmune diseases.
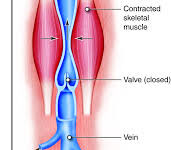
Despite these advancements, significant challenges remain. One major obstacle is vascularization, which is the process of developing a network of blood vessels that can supply oxygen and nutrients to bioprinted tissues. Without adequate blood supply, these tissues cannot survive post–implantation. Additionally, researchers are exploring methods to integrate bioprinted tissues with the human immune system to prevent rejection and ensure proper functionality once implanted. Another challenge is achieving the structural complexity and mechanical strength necessary for different organ types. Organs such as the heart and liver have intricate architectures that must be precisely replicated for them to function effectively. Also, the scalability of bioprinting is difficult, as current methods are often time–consuming and costly, limiting widespread clinical application.
The global shortage of donor organs emphasizes the urgent need for transformative solutions, and 3D bioprinting stands at the forefront of this revolution. This technology could eliminate the reliance on donors, drastically reduce transplant wait times, and provide personalized treatments tailored to individual patients. Although there are still major obstacles to overcome, each breakthrough brings the field closer to turning science fiction into reality. With relentless innovation and collaboration, 3D bioprinting has the potential not only to extend lives but to redefine the very nature of medicine, ushering in an era where no lives have to be lost waiting for an organ that technology can create.