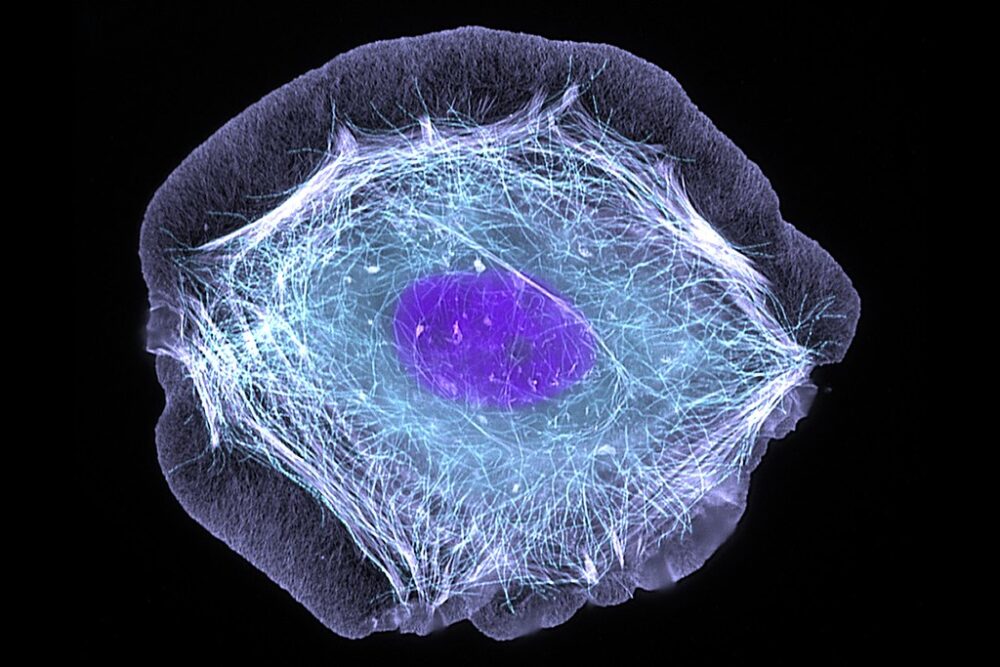
Apoptosis. Synonymous with the phrase “cell suicide,” it was initially discovered in 1842 by German scientist Carl Vogt. However, it wouldn’t be until 1972 that the now popularized term (from Greek, apo plus ptosis, or “falling off”) gained significance within the scientific community for the role it plays in fetal development, aging, and the formation of various neurodegenerative diseases such as Alzheimer’s and Parkinson’s.
Key discoveries on the subject of apoptosis have revealed that specific genes can control the induction or inhibition of cell death. While this effect was first observed in nematode worms, researchers have evidence to believe that similar genes responsible for the same function exist in the mammalian genome. Yet, the most significant discovery may be that apoptosis, despite its name, plays an integral role in the long-term survival of an organism. More specifically, apoptosis works to get rid of diseased cells that are damaged beyond repair. These cells, if allowed to live and replicate, would give rise to additional malformed cells with the potential to wreak havoc within the systems of an organism.
“Apoptosis, despite its name, plays an integral role in the long-term survival of an organism.”
If this sounds suspiciously similar to the mechanisms of cancer, that’s because it is. Cancer is a disease defined by the uncontrolled division of abnormal cells within a specific area of the body. In other words, cancer is what can happen when apoptosis doesn’t work properly. Being the second most common cause of death in the U.S., government funding for cancer research reached a whopping 6.8 billion dollars in 2022. Still, a conclusive cure has yet to be found. The search for answers becomes even more complicated because not all cancers are created equally. For example, while breast, testes, and skin cancers might be the most treatable if caught early enough, other cancers such as pancreatic, blood and bone (leukemia), and brain cancer are among the most difficult to cure. In particular, the outlook for glioblastoma, an aggressive and deadly brain cancer, is extremely poor, with only 25% of those who are diagnosed surviving past the first year.
Recently, however, a team of researchers found a promising new avenue for curing glioblastoma. While typical approaches to treating glioblastomas and other cancers may involve chemotherapy or surgical removal of tumors, the researchers focused primarily on targeting two key anti-apoptotic proteins commonly found in glioblastoma cells. These proteins — BCL-xL and MCL-1 — work to inhibit cell death in the glioblastoma cell, and as a result, allow the cancer to proliferate rapidly and without restriction. Yet, when the researchers specifically inhibited these proteins using chemotherapeutics called BH3-mimetics, the impact was significant — the glioblastoma tumors were not only reduced, but there were also no other significant negative effects as well.
Even more exciting? The findings aren’t just limited to glioblastomas; other cancer types can also benefit from a similar treatment approach. In fact, venetoclax, an FDA-approved drug that has a similar inhibitory function as BH3-mimetics, is already being used to treat blood cancers such as B-cell non-Hodgkin lymphomas. In a study looking at the impact of venetoclax on 28 blood cancer patients that hadn’t responded to other treatments, 75% of the patients were helped by the drug, with 21% experiencing complete remission.
Despite BH3-mimetics showing strong treatment potential, they have yet to be tested in clinical trials with human patients due to concerns with systemic toxicity (since anti-apoptotic proteins such as those in the BCL-2 family are also essential for platelet survival) and blood-brain barrier limitations. Future research may explore delivering BH3-mimetics more effectively through nanoparticle carriers or by modifying the surrounding tumor environment, seeking to enhance the drugs’ ability to target cancer while reducing harm to healthy, non-cancerous cells.
As advancements in drug delivery systems and tumor-targeting strategies continue to evolve, BH3-mimetics and other apoptosis-based therapies could offer new hope and better outcomes for patients with glioblastoma and other aggressive cancers.